Because it can be used with great accuracy, proton therapy is a particularly sparing form of radiation treatment with lower side effects. This kind of treatment is suitable above all for young cancer sufferers and for the treatment of tumours located close to radiation-sensitive organs.
Cancer and cancer therapies
Every third person develops a malignant tumour over the course of their life. In Switzerland, about 45,000 people face a cancer diagnosis every year. There are many different kinds of cancers. Many have become easier to cure than they were just a few years ago. Each kind of cancer reacts to certain kinds of therapy or to a specific combination of therapies.
The most important cancer therapies are:
- surgery (operation),
- radiation (also known as radiation therapy),
- drug-based therapy (such as chemotherapy, immunotherapy, anti-hormonal therapy).
More than half of all cancer patients receive radiation therapy in the course of their treatment. In most cases, radiation is combined with one other method of treatment: those affected are treated either before, during or after radiation with a second type of therapy. In some cases, even an inoperable tumour can be cured with radiation.
Like operations, radiation therapies belong to the category of local therapies. This means that the treatment targets only the tumour itself and possible side effects are limited to the affected area. Chemotherapies and other so-called systemic therapies are necessary when small clusters of tumour cells or metastases – cells that have detached themselves from the original tumour – need to be targeted and destroyed elsewhere in the body.
Radiation therapy
In radiation therapy, cancer is treated with the help of ionising radiation. Such radiation damages the genetic material located in the nucleus of the cancerous cell. As a result, the irradiated cancerous cell is unable to proliferate and subsequently dies.
Two kinds of ionized beams are used in cancer therapies: X-ray radiation or charged particles.
Traditional radiation oncology works with X-rays. However, more and more treatment centers are being established around the world where patients are treated with protons. The Paul Scherrer Institute is one of the pioneers of this comparatively new form of therapy. Protons are positively-charged particles, which is why these therapies are also referred to as particle radiation. Proton beams are the most common form of radiation used in particle therapy.
What are protons?
Protons are parts of atoms, just like neutrons and electrons. Neutrons and protons are found in the nucleus of an atom. Electrons are found in the atomic shell. Protons carry a positive electric charge. They constitute atoms, along with the uncharged neutrons and negatively-charged electrons. As the basic element of all solid, liquid and gaseous materials, atoms constitute the building blocks of all objects and living things.
The protons used for proton therapy at the PSI are extracted from hydrogen, the principal component of water. The hydrogen atom is the simplest of all atoms: it consists of only one proton and one electron and has no neutrons. The negatively-charged electrons are separated from the atomic nucleus of hydrogen atoms through a process of electrical discharge, leaving only the positively-charged protons. For the purposes of proton therapy, these remaining protons are subjected to rapid acceleration and are bundled into a beam form by a large, ring-shaped machine (cyclotron). The beam is then directed at the tumour. By the way: tiny amounts of hydrogen are needed for proton therapy: one course of treatment with 35 sessions requires only one sixth of a billionth of a gram. Or in other words: in theory, 1 gram of hydrogen would be enough to treat the entire world population with protons.
How protons work in the body
Like X-rays, proton beams damage the genetic make-up of cancerous cells, robbing those cells of the ability to proliferate, and eventually causing them to die off.
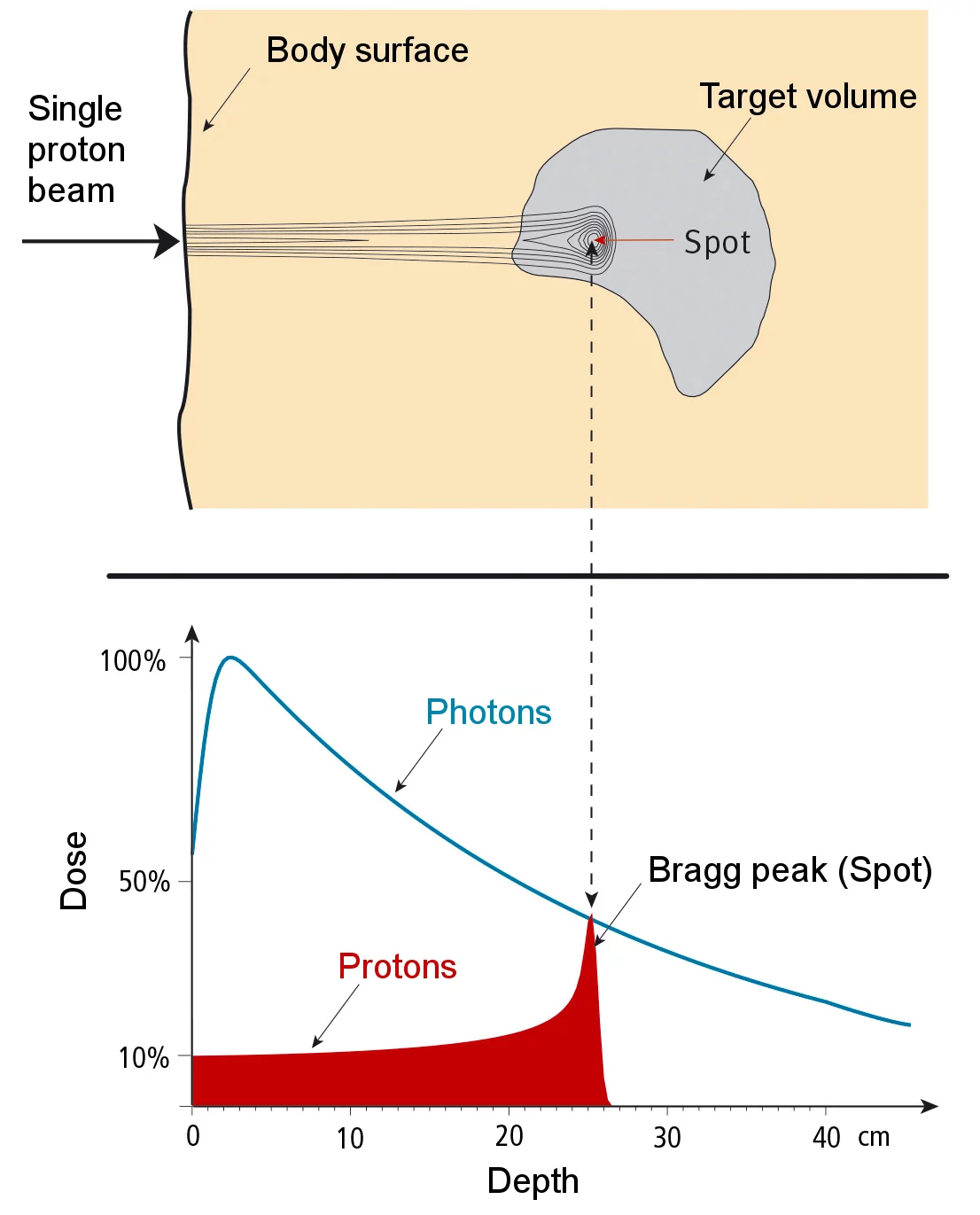
However, both kinds of radiation treatment affect not only cancerous cells but also healthy ones. Traditional radiation carried out with X-rays can’t avoid damaging the tissue surrounding a tumour. This side effect is significantly less pronounced during proton therapy. Surrounding tissue and vital organs are not harmed significantly. Proton beams give the most impact where they are most needed: in the tumour itself. The penetration depth of protons can be precisely calculated in advance, enabling the proton beam to develop maximum dosage within the area of the tumour. Most of the proton’s energy is released when the proton stops travelling at a spot called the Bragg peak, named after its discoverer William Henry Bragg. No radiation penetrates further than this spot. On its way from body surface to tumour the proton beam emits only small amounts of radiation into the healthy tissues, as can be seen in the diagram on the opposite page.
Proton therapy is only half as damaging to the body than a comparable dose of traditional radiation: neighbouring structures and sensitive organs such as the brain, the eyes, the spine, the heart or the intestines are not harmed as much. As a patient, you benefit from fewer side effects.
Radiation dose delivered by a pencil-thin proton beam penetrates body tissue to a specific depth determined by beam energy at point of entry.
In the top picture is a graphical representation of the dose distribution. In the bottom picture the proton dosage compared to the photon dosage (X-ray) as a function of depth.
The precision of proton therapy makes it possible to treat some cancers with higher radiation doses, improving a patient’s chances of being cured.
For which patients is proton therapy suitable?
In many countries, proton therapy is still considerably more expensive than conventional radiation therapy with photons. For this reason, the therapy is currently only considered for patients for whom significant advantages can be expected compared to conventional radiation therapy. In Switzerland, these cancers are listed on the so-called medical indication list (only in German, French and Italian) for proton therapy drawn up by the Bundesamt für Gesundheit (Federal Office of Public Health).
Children suffering from cancer are especially likely to benefit. The younger the patient the more important it is to minimize the long-term effects of radiation, including those for which the therapy might affect growth and development. The risk of developing secondary tumours in healthy tissue at a later stage (sometimes years or decades later) is minimised. This is why the Paul Scherrer Institute specialises in the radiation treatment of children.
At a glance: the advantages of proton therapy
- high precision tumour irradiation
- high radiation dose within the tumour with favourable dose distribution
- minimal damage to healthy cells of the body
- few side effects, good quality of life
- good, sustained chances of recovery