Proton therapy is a very complex, time and cost intensive form of radio-therapy. In Switzerland the health insurance providers, the Federal Health Agency (“Bundesamt für Gesundheit”) and PSI have agreed upon a list of indications which can be treated with proton therapy. Accordingly, only these listed diseases are treated at PSI. We cannot offer treatment for patients with other forms of tumors, nor with known metastases. Exceptions are made only for certain diseases in children and adolescents.
Ocular Tumors
By the end of 2024 we successfully treated over 8200 patients with ocular tumors. The prognosis after treatment is very good. In over 98% of all cases tumor growth was either permanently halted or the tumor actually disappeared over time. In more than 90%, the diseased eye could be rescued (Pica et al. 2023, Mouvet et al. 2019, Hennings et al. 2018, Via et al. 2018, Petrovic et al. 2014, Egger et al. 2003, Egger et al. 2001).
We also treat benign hemangiomas with 4x5 Gy(RBE).
Meningeomas
Over 250 patients treated at PSI suffered from a Meningioma. This tumor which usually does not metastasize develops from the membranes enveloping the brain (meninges). It grows between the skull bones and the surface of the brain, slowly displacing the brain volume. It can infiltrate the skull bones and the surrounding muscle tissues. Depending on the situation and size of the meningioma, it can cause symptoms such as intense headaches, epileptic seizures, brain deficiencies, consciousness disorder, paralysis and other neurological impairments. If the complete surgical removal of the tumor is not possible, radiation therapy could be indicated. Proton therapy is often appropriate for treating especially atypical (WHO Grade II) and malignant meningiomas (WHO Grad III) because a much higher dose is necessary than for the WHO Grade I meningiomas. Proton therapy enables a very precise spatial modulation of the radiation dose in the vicinity of sensitive structures, such as optical nerves (Krcek et al. 2023, Murray et al. 2017, Weber et al. 2012, Weber et al. 2004).
Low-grade glioma of the brain and spinal cord
Over 110 patients with low-grade brain tumors, so-called low-grade gliomas (LGG), have been treated with protons. These usually develop from glial cells, the supporting tissues of the brain. The closer these cells still resemble their source cells, the better the chances of the treatment’s success. In these cases, the tumors are classified as grade 1 and grade 2. According to the current stand of scientific knowledge, if a tumor has developed further away from its source cells – we call this dedifferentiation – proton therapy does not offer any better level of tumor control than modern photon irradiation with a linear accelerator. This is why grades 3 and 4 brain tumors, as well as glioblastoma multiforme, are not currently included in the PSI medical program. Usually the cases of such patients have been presented in neurology tumor boards before referral to PSI and discussion in our own proton therapy tumor board. This assures that the patient is offered the best possible form of therapy (Willmann et al. 2023, Badiyan et al. 2017).
Chondrosarcoma and chordoma of the skull base and spinal cord
Since 1996, over 670 patients have been treated with protons at PSI for chondrosarcoma or chordoma of the skull base or spinal cord. Many publications have resulted from our over 25 years of experience in treating these very rare tumors (Walser et al. 2021, Beer et al. 2020, Tran et al. 2019, Weber et al. 2018, Snider et al. 2018, Stieb et al. 2017, Weber et al. 2016, Schneider et al. 2013, Pehlivan et al. 2012, Staab et al. 2011, Ares et al. 2009, Weber et al. 2005).
This form of tumor develops in bone or connective tissues, or both. It grows slowly and metastasizes rarely, but destroys the usually sensitive and often vital neighboring structures. The proton beam penetrates tissues to a calculable depth, delivering the greatest, controlled dose of radiation at the end of the beam, the so-called Bragg Peak. This characteristic has been used now for many years to treat cordomas and chondrosarcomas of the skull base and spinal cord. Most of these cases were treated at the Harvard Cyclotron / Massachusetts General Hospital. In comparison to photon therapy, proton therapy has improved local tumor control rates for chondrosarcoma from approximately 40 % to over 80 % and for chordoma from less than 5 % to more than 50 %.
Developed at PSI, the IMPT technique (Intensity Modulated Proton Therapy) was implemented for the first time in 1999 to treat a young man with chondrosarcoma of the thoracic spine. This technique enabled the greatest possible protection of the spinal cord. Today, 20 years after completing the treatment, this patient is able to lead a completely normal life. This case illustrates clearly why chondrosarcoma and chordoma, besides melanoma of the eye, are considered clearly undisputed indications for proton therapy.
Sarcomas
Sarcomas are malignant cancers of the connective and supportive tissues. They can develop in all regions of the human body, for example in the pelvis, spine or in other bones and joints, as well as in muscle tissue. It requires a very high dose of radiation to treat them. By the end of 2024 we treated more than 410 sarcoma patients, usually after surgery or in combination with chemotherapy (Vazquez et al. 2023, Weber et al. 2017, Weber et al. 2015, Weber et al. 2007).
For tumors of the so-called soft tissue sarcoma type and diagnosed as inoperable or removable only through radical surgery which will result in a great loss of bodily function, PSI offers a course of pre-operative or definitive proton therapy in combination with hyperthermia therapy under the leadership of the Radio-Oncology Department of the Cantonal Hospital in Aarau. This treatment is offered within the framework of a prospective clinical trial (Short title: HYPROSAR, Trial description in the Clinicaltrials Registry), which has been approved by the Ethics Commission and is being carried out under close collaboration with the University Hospital of Zürich. All treatment requests from sarcoma patients or their referring physicians must be introduced with appropriate documentation at the sarcoma board of the Balgrist University Hospital in Zürich. A panel of experts will then decide if the patient is a suitable candidate for the trial. For further information, please contact Dr. Leiser (dominic.leiser@psi.ch) (Datta et al. 2016).
Head & Neck Tumors
Tumors of the ears, nose and throat areas (ENT tumors) often grow in close proximity to the sensitive structures of the brain, skull base and spine and require precise and sometimes large volume irradiation. Proton therapy lends itself very well for the treatment of these tumors; usually adenoid cystic carcinomas (ACC), benign and malignant parotid tumors, as well as nasopharynx tumors of different tumor tissue types. By the end of 2024 we treated more than 250 ENT tumors, some in conjunction with surgery, chemotherapy and, in a few cases, combined with conventional photon therapy.(<a href="/protontherapy/publikationen#walser2023">Walser et al. 2023</a>, <a href="/protontherapy/publikationen#pelak2020">Pelak et al. 2020</a>)
Pediatric Tumors
As of the end of 2024 we treated almost 900 children and adolescents between the ages of one and 18 years old. Since 2004 PSI has specialized in treating infants and small children. In collaboration with the Anesthesia Team of the Children’s Hospital of Zürich, more than 480 children between the ages of one and nine years were treated under sedation to overcome their inability to consciously cooperate due to their young age. At an average of 25 treatments per child, that adds up to more than 12000 anesthesia procedures carried out at PSI to date. The tumors, located in the head or torso, were treated with doses between 14.0 and 74.0 Gy(RBE), in a few cases in combination with conventional photon therapy. The largest groups of treated tumors were ependymoma, rhabdomyosarcoma, craniopharyngioma, medulloblastoma und Ewing’s sarcoma. These and other, more seldom tumors were often treated in combination with chemotherapy (Bojaxhiu et al. 2018, Weber et al. 2017, Leiser et al. 2016, Ares et al. 2016, Weber et al. 2015, Weber et al. 2015b, Thompson et al. 2013, Rombi et al. 2013).
At PSI almost all the children and adolescents are treated within the framework of a study or according to a study protocol. All are asked to participate in one prospective observation study:
- A survey of the quality of life after proton therapy (Pediatric Quality of Life = Pedqol questionnaire); a cooperative project with the University of Bonn in Germany;
Focal point children, adolescents and young people
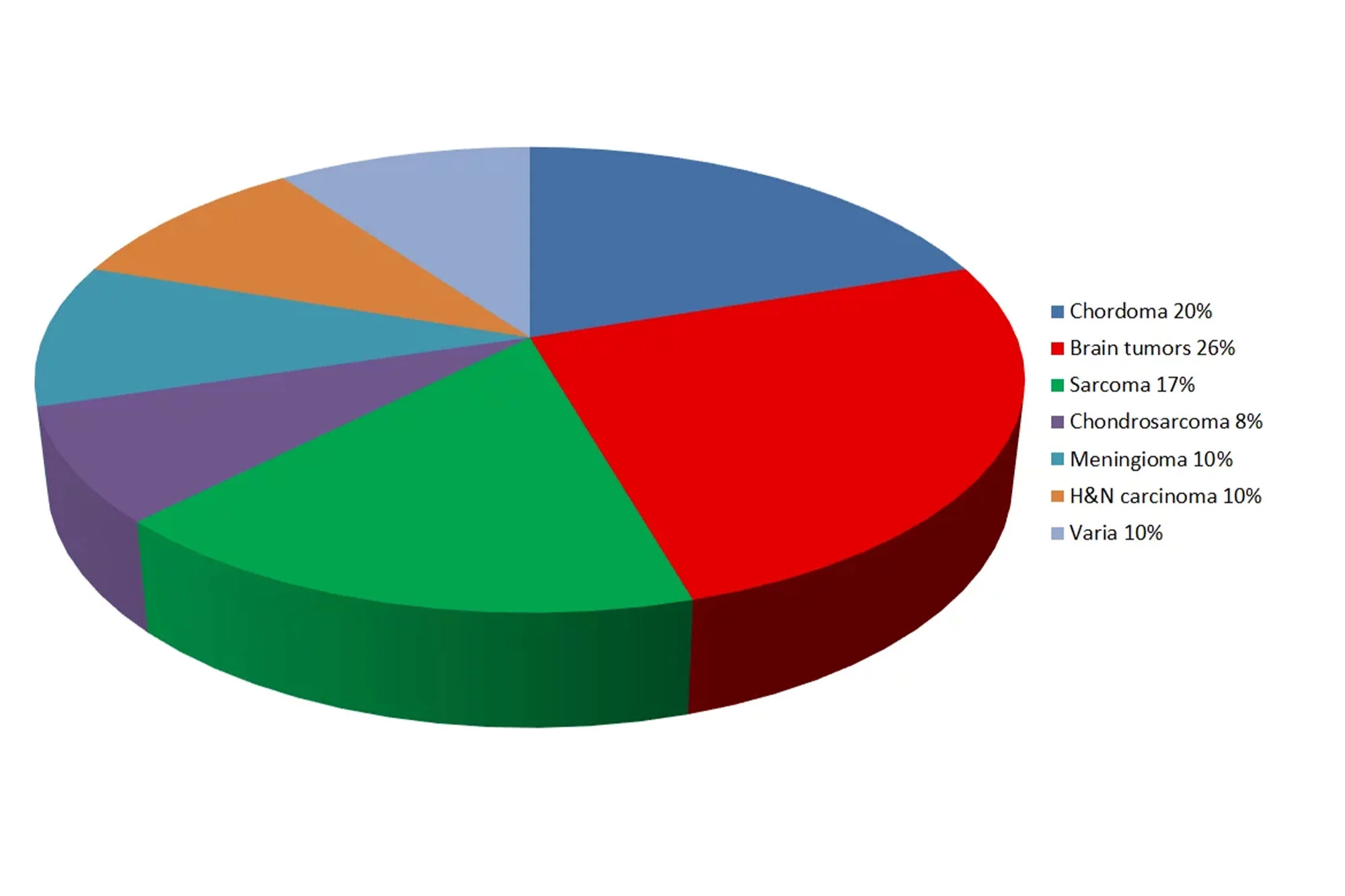
The age distribution of our patients earns special attention: Almost 60% are younger than 40 years of age and approximately 35% are children or adolescents under the age of 18. These patients can especially profit from the precise application of the radiation dose within the tumor and only low dose to the tissues outside of the targeted volume. This means that the growing and very sensitive juvenile organism is much better shielded in comparison to photon therapy, thereby lowering the probability of subsequent secondary tumors.