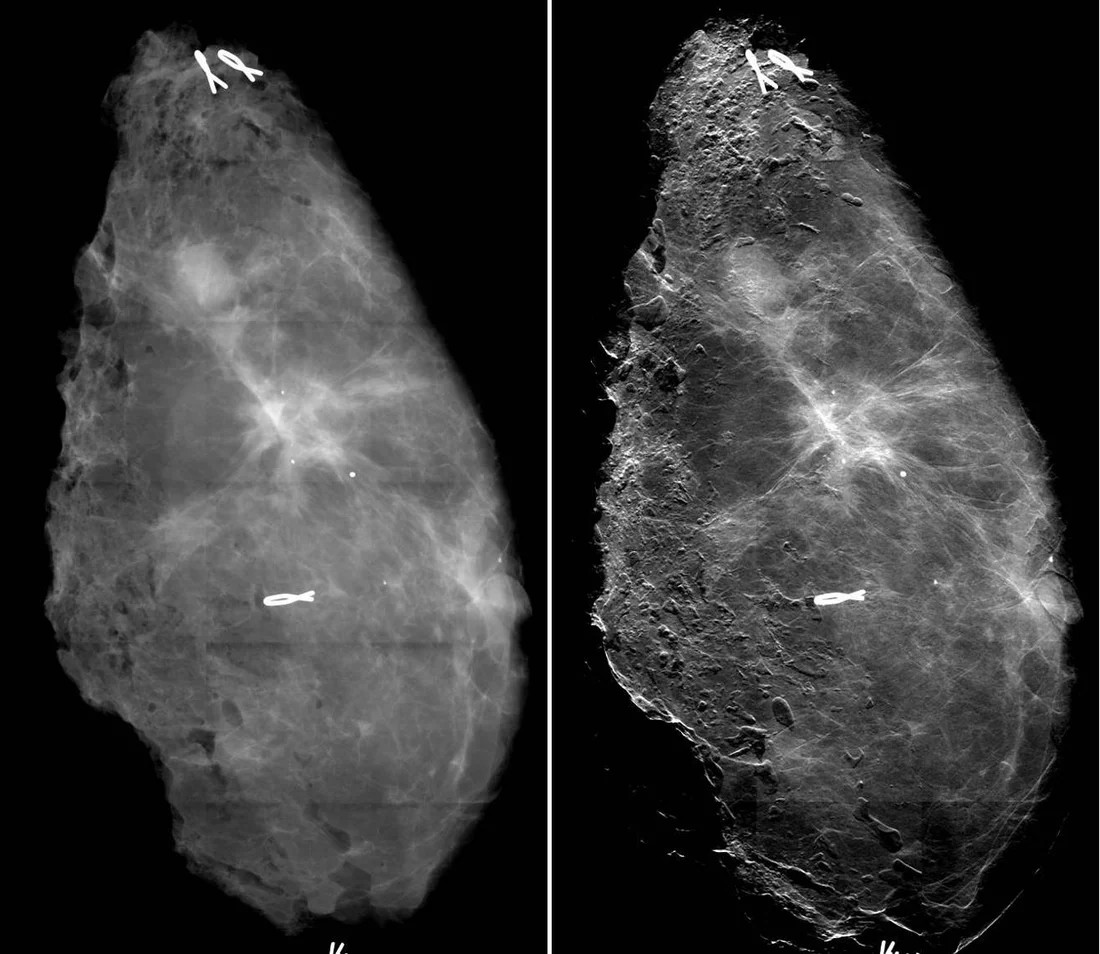
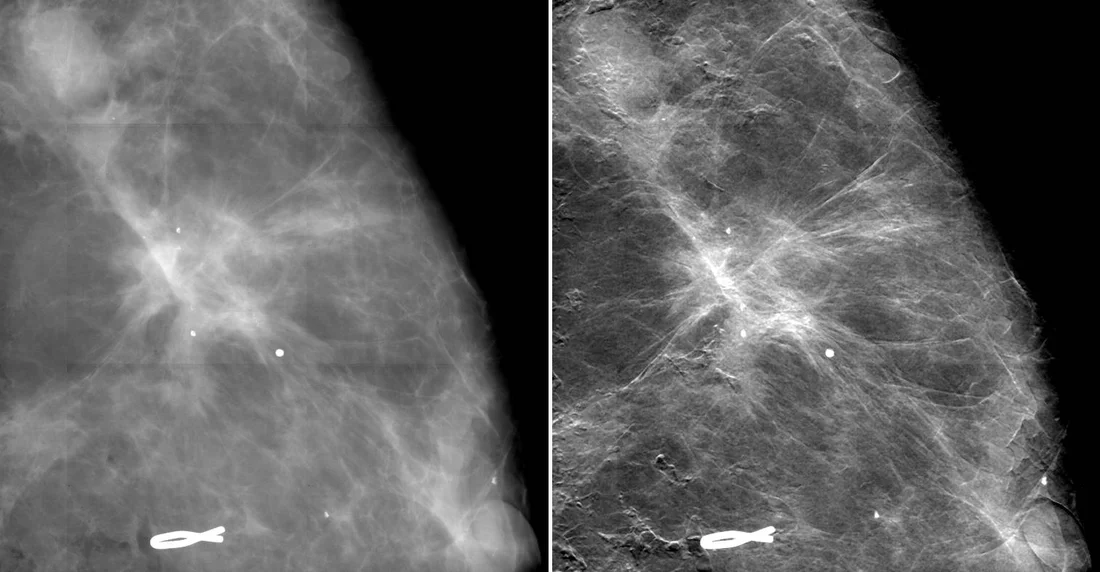
According to a study that has just been published, a novel mammography procedure developed at the Paul Scherrer Institute (PSI), in cooperation with the Certified Breast Centre of the Kantonsspital Baden and the industrial partner Philips, could generate substantial added-value for the diagnosis of breast cancer in medical practice. The innovative mammography procedure draws on the fact that as x-rays pass through tissue, they are not only absorbed but also refracted. This additional refraction information contributes to a clearer, more detailed image of the breast and renders even the tiniest tissue changes visible. For this study, international breast experts compared standard mammograms of recently resected breast tissue to images produced using the new method, and the results were very positive. According to the authors of the study, the new image quality not only leads to a more accurate diagnosis of breast cancer, but it could also improve early detection.
Study highlights the benefits of innovative mammography procedure
The study, published in the scientific journal “Investigative Radiology”, evaluated the imaging quality and the potential clinical relevance of the new methodology. To this end, experienced radiologists compared the quality of normal mammograms with those of the innovative method. Evaluating the breast tissue of 33 patients who had recently undergone surgery, the experts agreed that the new images were of far better quality than traditional mammogram images. Thus, such a technique could constitute a significant advancement for the diagnosis of breast cancer.
Potential early detection of breast cancer
When imaging a women’s breast with the innovative technique, the demarcation between tumour tissue and healthy tissue is better identified. Even the fine extensions of the growth are distinctly recognisable. “This may mean it is possible to better prepare for an operation and to determine the surgical area more accurately”, explains Nik Hauser, Director of the Certified Breast Centre at the Kantonsspital Baden. Small white flecks are also visible in the images. These microcalcifications provide information about the malignancy of changes in breast tissue depending on their sizes and structures. As the increased image sharpness already makes many smaller structures of this kind visible, breast cancer could also be detected at a very early pre-stage. “This is extremely promising in practice”, says Hauser, since “the earlier we detect and treat a suspicious change in tissue, the greater the chances of survival”. * Exploiting the additional information available*
In conventional mammography, one measures how much of the radiation passes through the breast tissue and how much is retained. This ratio depends on the nature of the tissue, and very often it shows little variations making discrimination between tumours and healthy tissue very difficult. However, when X-rays pass through tissue, they are not only attenuated but also slightly modified in their direction. This additional information can be retrieved in the images generated by the new technique and contributes to increasing contrast and feature delineation in the new mammograms. PSI has been pioneering this technique for many years. “Instead of just measuring their absorption, we worked out how to record the refraction and scattering of the x-rays as well”, explains Marco Stampanoni, leader of the project at PSI and professor at the ETH Zurich. Another advantage is that these significantly improved images can theoretically be obtained with the same x-ray dose as with the conventional mammogram. “We are working very hard on this aspect, since this is crucial for the implementation of our approach into clinical devices”, clarifies Stampanoni. * Plans for study involving breast cancer patients*
Maintaining a small dose is important because the x-ray exposure of the body must be kept to a minimum. In order to introduce this method in practice, studies in patients must compare the innovative method with the standard method used today. To this end, in a next study, patients with a previously diagnosed malignant breast tumour will be examined again with a mammogram obtained with the new method. For those patients, the enhanced images could potentially improve the subsequent treatment.
“On the home stretch”
“We have already covered a significant part of the road towards the implementation of the new technology in practice – we’re on the home stretch now”, says Marco Stampanoni. “As a next step, we want to validate the new mammography procedure in patients.” The team has great expectations of the first tests with the novel technique and is convinced that this technology will become established. “Once it is available, it will quickly gain acceptance”, reckons Hauser.
Text: Simone Nägeli
About PSI
The Paul Scherrer Institute develops, builds and operates large, complex research facilities, and makes them available to the national and international research community. The Institute's own key research priorities are in the investigation of matter and material, energy and the environment; and human health. PSI is Switzerland's largest research institution, with 1500 members of staff and an annual budget of approximately 300 million CHF.
Contact
Prof. Dr. Marco StampanoniInstitute for Biomedical Engineering at ETH Zurich and the Laboratory for Macromolecules
and Imaging at the Paul Scherrer Institute, 5232 Villigen PSI, Switzerland
Tel.: +41 563 104 724 or +41 (0) 446 328 650
Email: marco.stampanoni@psi.ch or stampanoni@biomed.ee.ethz.ch [German, English, Italian, French]
Dr. Nik Hauser
Deputy Chief Medical Officer at the Women’s Clinic and Director of the Certified Breast Centre Baden AG, CH-5404 Baden
Tel.: +41 564 863 636, Email: nik.hauser@ksb.ch [German, English]
Original Publication
A Study on Mastectomy Samples to Evaluate Breast Imaging Quality and Potential Clinical Relevance of Differential Phase Contrast MammographyHauser, Nik; Kubik-Huch, Rahel A.; Wang, Zhentian; Trippel, Mafalda; Singer, Gad; Hohl, Michael K.; Roessl, Ewald; Wieberneit, Nataly; Köhler, Thomas; van Stevendaal, Udo; Stampanoni, Marco
Investigative Radiology;
DOI: 10.1097/RLI.0000000000000001