Better than CT and MRI: researchers at the Inselspital Berne, the University Hospital Basel and the Paul Scherrer Institute have devised a new method to detect small tumours in the pancreas.
Swiss researchers have developed a method that is able to reliably localise certain tumours in the pancreas known as insulinomas. The new method was presented online in the renowned medical journal Lancet on 25 July. The print publication is due to follow in September. The study has been supported by the Swiss National Science Foundation, the Swiss Cancer League and the United Kingdom’s Department of Health.
Dangerously low blood sugar levels
Insulinomas are rare tumours that produce hormones, especially insulin. They are normally found in the pancreas and are mostly benign and small (approx. 1 to 1.5 cm in diameter). As they release insulin uncontrollably, however, they repeatedly cause dangerously low blood sugar levels (hypoglycaemia), which can lead to disorientation, loss of consciousness and in rare cases to seizures or coma. They often take a long time to be diagnosed. For the patients, this means a prolonged and intensive period of suffering.
Operate – but where?
The only cure is to remove the insulinoma by a surgical intervention. However, the surgeon needs to know the exact location of the insulinoma. Using conventional imaging such as CT (computed tomography) and MRI (magnetic resonance imaging), only sixty to seventy per cent of these tumours can be located, which means thirty to forty per cent cannot be identified. So far, invasive investigations are proposed in case of a negative outcome of conventional imaging: these include insulin concentration measurements in the vessels surrounding the pancreas. For this purpose, a catheter has to be inserted into the pancreatic vessels and the liver vein. Alternatively, a gastroscopy including an ultrasound investigation of the pancreas is performed in order to detect smaller tumours.
Tumour made visible radioactively
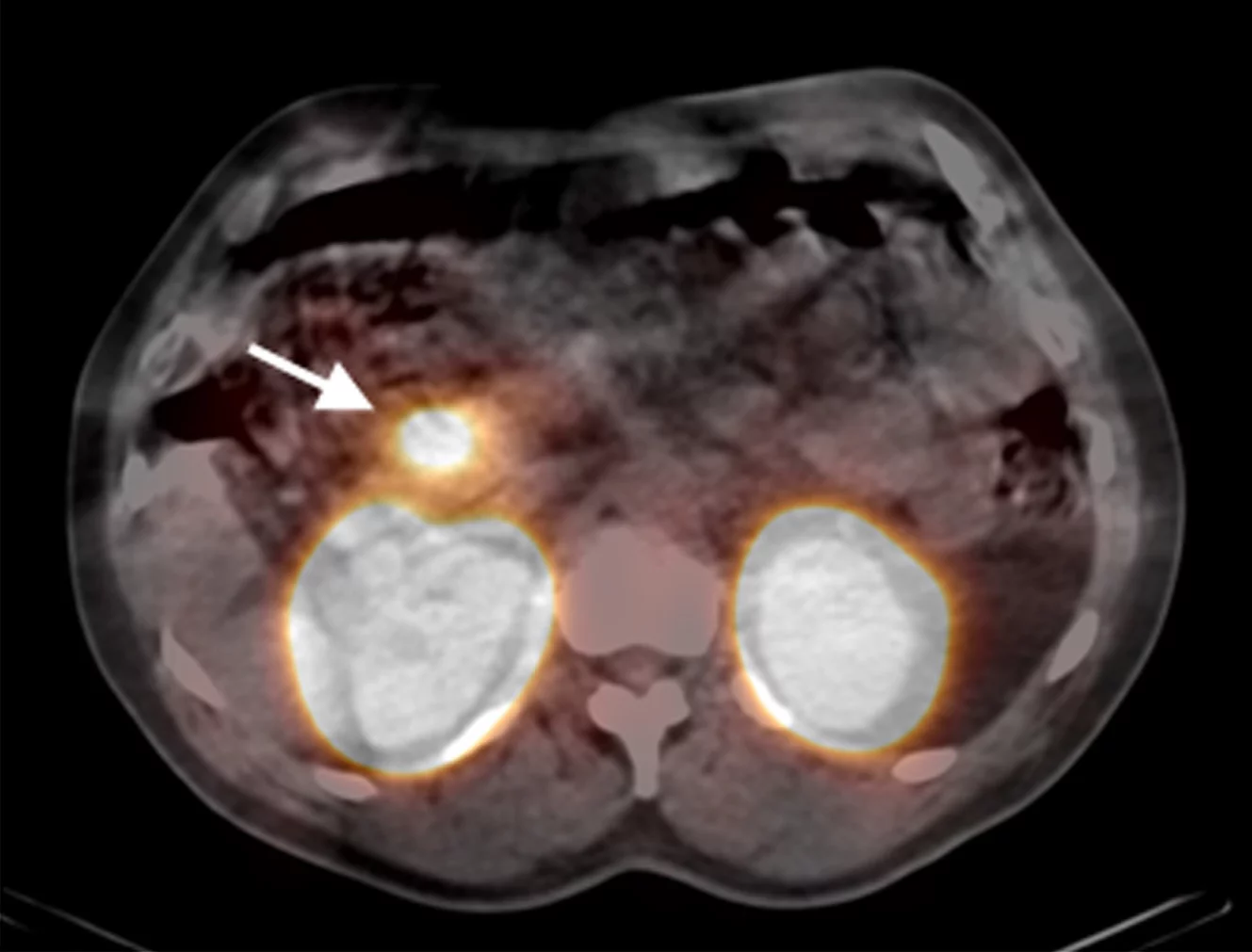
In order to localize the insulinomas, the researchers injected an artificial substance combined with low-level radioactive indium into thirty patients with a strong suspicion of insulinomas. The substance accumulates in the tumour and, thanks to its low-level radioactive radiation, renders the mini-tumour visible in a special camera. As a result, ninety-five per cent of the insulinomas could be localised. With CT or MRI, the detection rate would only have been forty-seven per cent. “It is likely that this method will replace the existing invasive methods for locating insulinomas in the future,” says Professor Emanuel Christ from the Inselspital Berne, the endocrinologist (metabolism specialist) responsible for this research project.
Success thanks to international network
What might sound simple was only possible thanks to years of pioneering work and a national and international research network: at the Inselspital and the University Hospital Basel, Christ, nuclear medicine researcher Professor Damian Wild and private lecturer Flavio Forrer defined the aim of the study, the study method and the criteria for patient selection. Together with colleagues in St. Gallen, Lucerne, Freiburg im Breisgau (Germany) and London, they then selected patients for the study. In a proof-of-concept study, the researchers successfully investigated six Swiss patients in 2009. The aim of this subsequent prospective large-scale study was to confirm the results.
Tumour outsmarted with keyhole technique
Dr Martin Béhé (now at the Paul Scherrer Institute) and colleagues developed the low-level radioactive substance to outwit the invisible tumour by exploiting a familiar phenomenon: nearly all insulinomas have a large number of so-called GLP-1 receptors on their surface – a kind of keyhole that can only be opened with a single key, the chemical substance GLP-1. The researchers used a similar substance they had co-developed, exendin-4, which fits the same “keyhole”. Using exendin-4, the low-level radioactive indium could thus be smuggled into the tumour and its veil of camouflage lifted.
Text: Inselspital Bern, Universitätsspital Basel, PSI
About PSI
The Paul Scherrer Institute develops, builds and operates large, complex research facilities, and makes them available to the national and international research community. The Institute's own key research priorities are in the investigation of matter and material, energy and the environment; and human health. PSI is Switzerland's largest research institution, with 1500 members of staff and an annual budget of approximately 300 million CHF.
Contact
Prof. Dr. Emanuel Christ, Inselspital, Universitätsspital Bern, Universitätspoliklinik für Endokrinologie, Diabetologie und Klinische Ernährung,E-Mail: Emanuel.Christ@insel.ch
Prof. Dr. Damian Wild, Universitätsspital Basel, Abteilung für Nuklearmedizin / Universitätsklinikum Freiburg / University College London Hospital,
E-Mail: Damian.Wild@usb.ch
Dr. Martin Béhé, Paul Scherrer Institut, Zentrum für radiopharmazeutische Wissenschaft / Universitätsklinikum Freiburg,
Phone: 056 310 28 17, E-Mail: martin.behe@psi.ch
Original Publication
Glucagon-like peptide-1 receptor imaging for the localisation of insulinomas: a prospective multicentre imaging studyProf Emanuel Christ, Prof Damian Wild, Susanne Ederer, Martin Béhé PhD, Guillaume Nicolas, Prof Martyn E Caplin, Prof Michael Brändle, Thomas Clerici, Stefan Fischli, Prof Christoph Stettler, Prof Peter J Ell, Prof Jochen Seufert, Prof Beat Gloor, Prof Aurel Perren, Prof Jean Claude Reubi, Flavio Forrer
The Lancet Diabetes & Endocrinology, Early Online Publication, 25 July 2013
http://www.thelancet.com/journals/landia/onlinefirst