Which people are especially susceptible to infection by Sars-CoV-2? How can proteins of the virus be most effectively disabled? And why are some virus mutants so much more infectious than the original variant? In Covid-19 research, the Paul Scherrer Institute PSI is exploring many different avenues to find answers to these and other questions.
In November 2020, a mutated variant of the novel coronavirus Sars-CoV-2 spread in southeast England. The media christened it the Kent or British variant; scientifically it is known as lineage B.1.1.7 and according to new WHO nomenclature, it is the Alpha variant. It quickly became clear that this mutant is roughly 1.6 times more contagious than the original coronavirus. Shortly afterwards, other variants were discovered, for example the Beta variant in South Africa and now the Delta variant in India.
All concerning variants of the virus have one thing in common: changes in the area of the virus's hereditary material that contains the blueprint for an important protein, the spike protein. This protein sits on the surface of the virus and serves as a kind of gripping arm that enables the pathogen to dock onto human cells, in order to subsequently infect them.
Proteins like the spike protein consist of a sequence of different building blocks, the amino acids. Not every amino acid has the same significance for the functionality of the protein. In early summer 2020, researchers in Berlin, with support from PSI, used computer models to determine which amino acids in the spike protein are particularly important for the virus. It was shown that position 501 – along with a few other places – is virtually predestined to be changed by mutations. "Later, N501Y was discovered to be one the key mutations in the coronavirus variants that had developed," says Gebhard Schertler, head of the Biology and Chemistry Division at PSI and co-author of the study. Due to the mutation, a different amino acid is incorporated at position 501 of the protein, thereby strengthening the binding to the receptor. Alpha, Beta as well as Gamma carry this mutation.
That study is impressive proof of how well the development of the virus can be predicted if scientists know the structures of its components as well as the counterparts in human cells that are involved in the infection process.
Coronavirus proteins made in Villigen
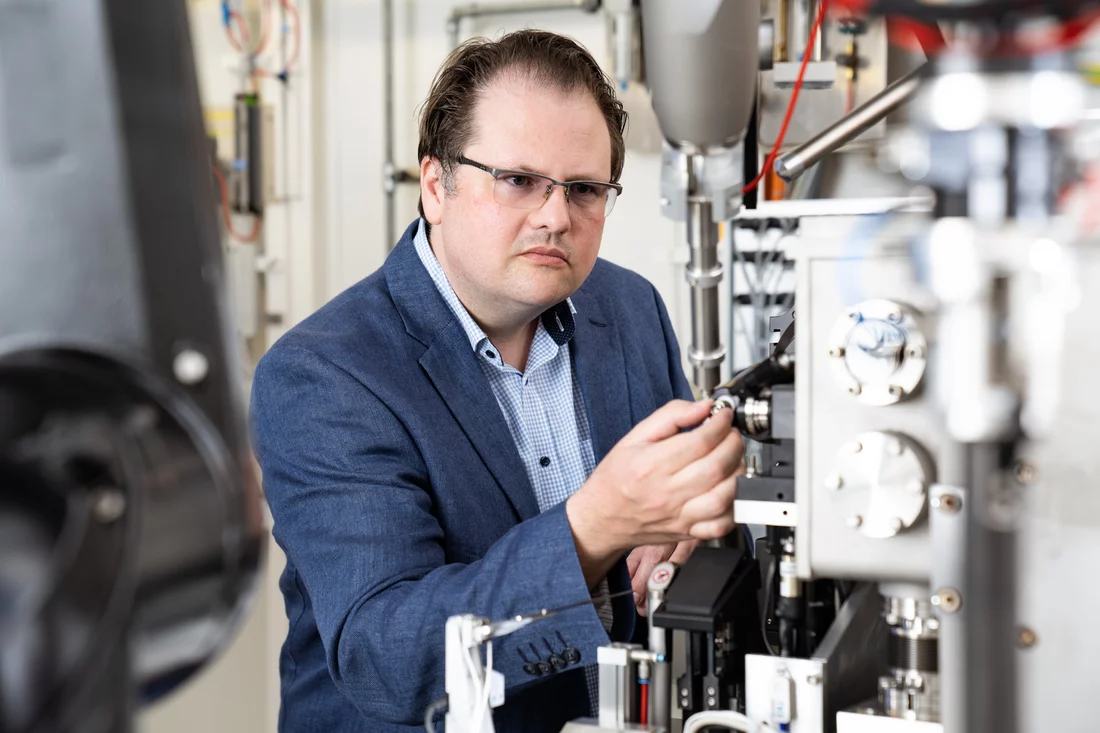
In PSI's Laboratory of Nanoscale Biology, molecular biologist Roger Benoit is also working on mutants of the coronavirus. He wants to understand the molecular details that make certain virus variants more infectious than others. To do this, he produces proteins in the laboratory that have been changed by gene mutations and investigates how they bind to the receptor.
Benoit has published instructions on how to produce part of the spike protein in cell cultures in the laboratory using simple means. For many coronavirus researchers worldwide, these virus proteins are a sought-after resource, because they can be studied safely in the laboratory; scientists need not work with the complete, infectious virus. "My goal was for everyone doing research on the coronavirus to be able to produce this protein themselves – even in the smallest cell culture laboratory," says the PSI researcher.
Tests have confirmed that Benoit's production method works. "I get inquiries about my production method almost weekly from the worldwide research community," he says.
Benoit is not the only one at PSI who knows how to produce coronavirus proteins. "We've been working with very challenging proteins here for many years," says Jacopo Marino, a postdoc in the PSI Laboratory of Biomolecular Research. With a team, he produced the nucleocapsid protein. This protein forms a protective shell around the genetic material of the virus and thus is essential for its function and reproduction. In large-scale antibody tests using the protein produced at PSI, the University Hospital of Zurich is investigating how many people in Switzerland have actually been infected with the virus – that is, how high the number of unreported coronavirus cases is.
Gateway into the cell
Sars-CoV-2 uses a very specific protein as the entry point into the human cell: the so-called angiotensin-converting enzyme 2, or ACE2 for short. Many cells in the human body form this protein on their surface; the virus docks on it and thus gains access. So, without ACE2 there is no infection.
Nevertheless, much remains unknown about the ACE2 protein. Where in the body does it sit exactly, and above all: How do previous illnesses or the use of medication change its occurrence in the body? Does its distribution differ between men and women?
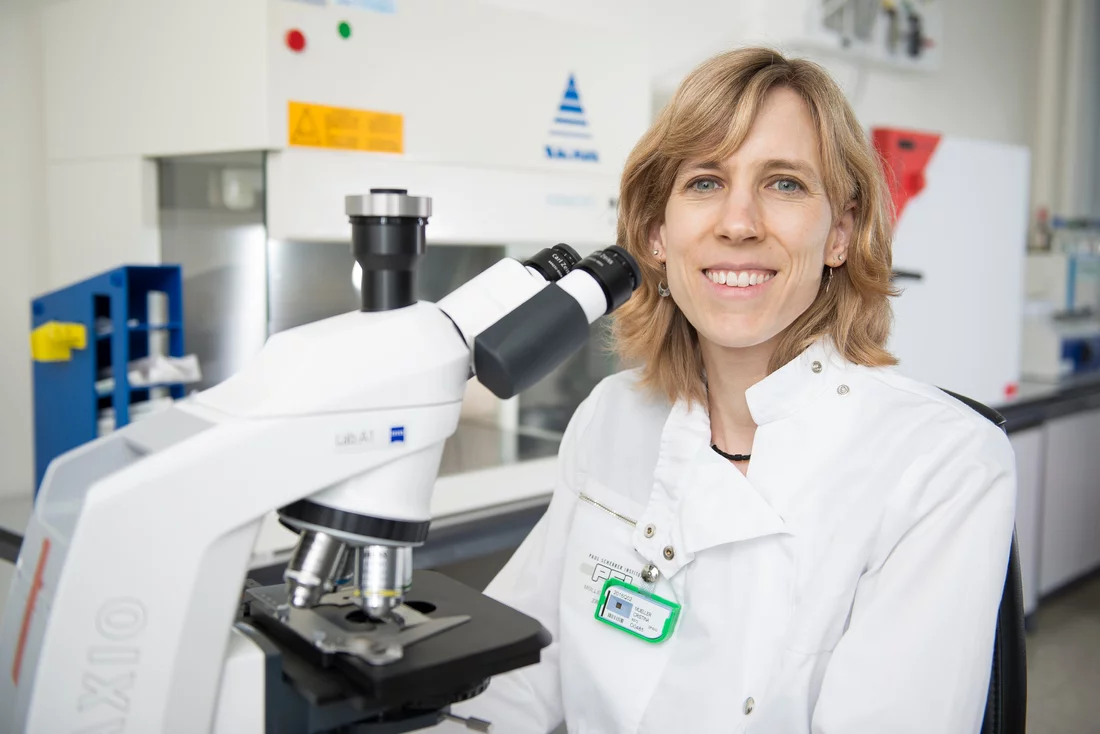
Cristina Müller of the Center for Radiopharmaceutical Sciences wants to address these questions. She is using a diagnostic method to show how and in which organs of the body ACE2 is built. "Then it would also be possible to investigate which impact it has on the susceptibility to infection or the severity of the course of the disease," she says. "For example, is it good or bad if someone produces a lot of ACE2 molecules?"
To answer this question, Cristina Müller wants to use the imaging method of positron emission tomography: This process generates three-dimensional images of living organisms by making the distribution of a radiolabelled substance visible in the body. Müller and her team are in the process of developing such a substance – called a radiotracer. "In cell culture and in animal experiments, we have seen that a first variant of one such radiotracer binds selectively to ACE2 – and really only to it," says Cristina Müller. Now it's a matter of further optimising the radiotracer to make it bind better to ACE so that the protein is more visible. The goal is to enable using the substance in humans soon.
In this project too, models have contributed to success: Xavier Deupi of the Laboratory of Scientific Computing and Modelling investigated on the computer how the substance binds to ACE2. That made it possible to estimate where this can best be changed for a radioactive label without impairing the binding to ACE2.
It also pays to take a detailed look at human lung tissue with regard to Covid-19. In a project with the University of Bern, Marco Stampanoni of the Laboratory of Macromolecules and Bioimaging is examining lung tissue. The lungs of a person infected with the coronavirus not only suffer from the infection itself, but also often from the violent reaction of the immune system, which causes water and immune cells to accumulate in the alveoli. This is a major reason why, if the course of the infection is severe, patients can no longer breathe adequately. Stampanoni's long-term goal is to develop new diagnostic techniques for early diagnosis or personalised follow-up examinations.
Which cells does the coronavirus hijack?
The older you are, the higher your risk of dying from an infection with the coronavirus. G.V. Shivashankar, head of the Laboratory of Nanoscale Biology, together with collaboration partner Caroline Uhler from MIT in the USA, has developed a remarkable hypothesis: The stiffness of cells should play a decisive role in the course of the disease – and with age, the stiffness of lung cells, for example, increases. According to this hypothesis, coronaviruses can multiply much better in older cells. On the basis of this hypothesis, Shivashankar and Uhler identified the first active ingredients that are on the market for the treatment of other diseases but should also help against Covid-19. "Surprisingly, we found out that clinical studies on one of the drug groups are already running with Covid-19 patients," Shivashankar says. "So we will soon know whether these drugs actually help."
Researchers have also observed that the coronavirus selectively affects those cells in the respiratory tract that possess cilia. Cilia are long cell processes that move back and forth through mucus and thus sweep bacteria, viruses, and dust out of the airways. In the early infection phase, coronaviruses penetrate the airways through the cells of the cilia. However, it is not yet known what role the cilia play: Do they attract the viruses? Do they serve as a kind of scaffolding through which they can enter the cells? Do the viruses hijack the cilia?
Takashi Ishikawa, also from the Laboratory of Nanoscale Biology, is pursuing this question. Together with Roger Benoit, he grows cells from human bronchi. Starting with a carpet of these cells with cilia, he adds coronaviruses that are genetically modified in such a way that they can still infect human cells, but can no longer multiply in them. "In this way, we want to precisely observe the entry mechanism using an electron microscope." Ishikawa hopes his findings will then help identify risk groups or even develop a drug.
X-raying and disabling proteins
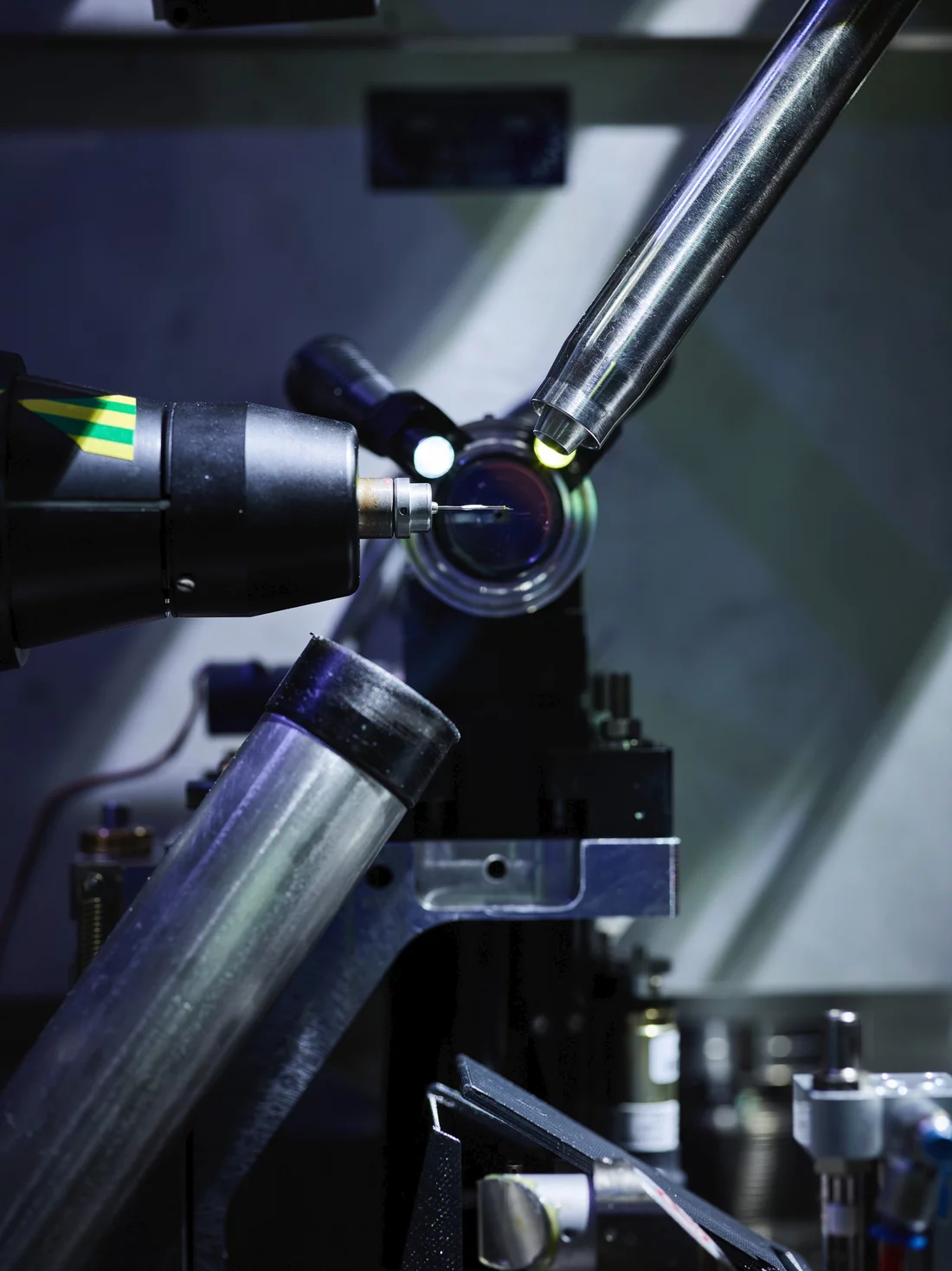
Deciphering the structure of proteins is a specialty of PSI. With X-rays from the Swiss Light Source SLS, tiny components of the virus can be viewed at the level of individual atoms. Three experiment stations on the beamlines of PSI's Macromolecular Crystallography Group have been used for this for many years. If you know the exact structure of a virus protein, you can search for the right medical active ingredients or assemble them chemically.
Measurements related to Covid-19 have been given priority at SLS since the beginning of the pandemic. One of the first scientists to apply for measurement time was Donghyuk Shin from the Goethe University in Frankfurt. At SLS he deciphered the structure of the virus protein PLpro (papain-like protease) and identified it as a possible target for future drugs. If you can block this protein, you can slow down virus production and at the same time strengthen the human cells' innate immune response, so that the body may then be able to defend itself against the virus on its own.
Other coronavirus proteins that have been X-rayed at SLS are the macrodomain and the nucleocapsid protein. In collaboration with coronavirus expert Sheng Cui at the Chinese Academy of Medical Sciences, Meitian Wang's team from the PSI Laboratory for Macromolecules and Bioimaging is examining a helicase, another potential target for drugs against Covid-19. This enzyme ensures that the genetic material of the virus can multiply in the cells of an infected person.
The researchers are also trying to find substances that can bind to the virus proteins and block them. In doing so, they allow possible active ingredients to act on crystals of the virus proteins. A subsequent structure determination at SLS reveals whether the molecules have bound to the protein and if so, where. In the relatively new method known as fragment screening, only fragments of molecules that are typical for promising active ingredients are added, instead of complete active ingredients. From the many individual items of information, the researchers hope to arrive at an answer to what an effective drug might look like.
Researchers at PSI are also testing the 3CL protease to identify possible inhibitors. After replication, this virus enzyme cuts the virus's own proteins so that new coronaviruses capable of reproduction arise. "The 3CL protease is a very promising drug target on the coronavirus," says Meitian Wang. "The virus cannot function without this protein."
The studies on this protein are being carried out in collaboration with the pharmaceutical company Idorsia and other research groups, for example at the University in Groningen in the Netherlands. "It normally takes ten to fifteen years to develop a new drug," says Wang. "But now that so many researchers are pursuing the same goal, we are probably moving somewhat faster."
With all these activities, researchers at PSI are making important contributions to better understanding the new Sars-CoV-2 virus and developing effective strategies to prevent it from spreading and to treat infected people. This case also highlights the elementary prerequisites for such advances: networking within the top-level research community worldwide, the complex and extremely powerful facilities at PSI, and the excellent researchers who work in Switzerland and at PSI.
Text: Paul Scherrer Institute/Brigitte Osterath
Contact
Dr. Roger Benoit
Laboratory of Nanoscale Biology
Paul Scherrer Institute, Forschungsstrasse 111, 5232 Villigen PSI, Switzerland
Telephone: +41 56 310 47 03, e-mail: roger.benoit@psi.ch [German, English]
Prof. Dr. Takashi Ishikawa
Laboratory of Nanoscale Biology
Paul Scherrer Institute, Forschungsstrasse 111, 5232 Villigen PSI, Switzerland
Telephone: +41 56 310 42 17, e-mail: takashi.ishikawa@psi.ch [English, Japanese]
PD Dr. Cristina Müller
Center for Radiopharmaceutical Sciences
Paul Scherrer Institute, Forschungsstrasse 111, 5232 Villigen PSI, Switzerland
Telephone: +41 56 310 44 54, e-mail: cristina.mueller@psi.ch [German, English]
Prof. Dr. Gebhard Schertler
Head of the Biology and Chemistry Division
Paul Scherrer Institute, Forschungsstrasse 111, 5232 Villigen PSI, Switzerland
Telephone: +41 56 310 42 65, e-mail: gebhard.schertler@psi.ch [German, English]
Prof. Dr. G.V. Shivashankar
Head of the Laboratory of Nanoscale Biology
Paul Scherrer Institute, Forschungsstrasse 111, 5232 Villigen PSI, Switzerland
Telephone: +41 56 310 42 50, e-mail: gv.shivashankar@psi.ch [English]
Dr. Meitian Wang
Laboratory for Macromolecules and Bioimaging
Paul Scherrer Institute, Forschungsstrasse 111, 5232 Villigen PSI, Switzerland
Telephone: +41 56 310 41 75, e-mail: meitian.wang@psi.ch [English, Chinese]
Further information
- Research on Covid-19 at PSI
- Why Covid-19 hits older people especially hard
- Covid-19 research: Anti-viral strategy with double effect
- A question of binding
Selected original publications
A graph-based approach identifies dynamic H-bond communication networks in spike protein S of SARS-CoV-2
K. Karathanou, M. Lazaratos, É. Bertalan, M. Siemers, K. Buzar, G.F.X. Schertler, C. del Val, A.-N. Bondar,
Journal of Structural Biology, 10. September 2020 (online)
DOI: 10.1016/j.jsb.2020.107617
Design, Expression, Purification, and Characterization of a YFP-Tagged 2019-nCoV Spike Receptor-Binding Domain Construct
T. Bierig, G. Collu, A. Blanc, E. Poghosyan, R. M. Benoit
Frontiers in Bioengineering and Biotechnology, 21. Dezember 2020 (online)
DOI: 10.3389/fbioe.2020.618615
SARS-CoV-2 expression and aging to identify candidates for drug repurposing
A. Belyaeva, L. Cammarata, A. Radhakrishnan, C. Squires, K. Dai Yang, G. V. Shivashankar, C. Uhler
Nature Communications, 15 February 2021 (online)
DOI: 10.1038/s41467-021-21056-z
Mechano-genomic regulation of coronaviruses and its interplay with ageing
C. Uhler, G. V. Shivashankar
Nature Reviews Molecular Cell Biology, 02 April 2020 (online)
DOI: 10.1038/s41580-020-0242-z
Papain-like protease regulates SARS-CoV-2 viral spread and innate immunity
D. Shin, R. Mukherjee, D. Grewe, D. Bojkova, K. Baek, A. Bhattacharya, L. Schulz, M. Widera, A. R. Mehdipour, G. Tascher, K.-P.
Knobeloch, K. Rajalingam, H. Ovaa, B. Schulman, J. Cinatl, G. Hummer, S. Ciesek, I. Dikic
Nature, 29 July 2020 (online)
DOI: 10.1038/s41586-020-2601-5
Crystal structure of SARS-CoV-2 papain-like protease
X. Gao, B. Qin, P. Chen, K. Zhu, P. Hou, J.A. Wojdyla, M. Wang, S. Cui
Acta Pharmaceutica Sinica B, 2 September 2020 (online)
DOI: 10.1016/j.apsb.2020.08.014
Combining High-Throughput Synthesis and High-Throughput Protein Crystallography for Accelerated Hit Identification
A. Doemling, F. Sutanto, S. Shaabani, R. Oerlemans, E. Deniz, P. Patil, M. Hadian, M. Wang, M.E. Sharpe, M.R. Groves
Angewandte Chemie International Edition, 7 June 2021 (online)
DOI: 10.1002/anie.202105584
Copyright
PSI provides image and/or video material free of charge for media coverage of the content of the above text. Use of this material for other purposes is not permitted. This also includes the transfer of the image and video material into databases as well as sale by third parties.