In the laboratories of PSI, researchers are producing proteins of the novel coronavirus Sars-CoV-2. The University Hospital of Zurich is using these in a long-term study to investigate how many people in Switzerland have actually been infected with the virus.
It's March 2020 – the month the world changed forever: It has become clear to experts that the spread of the novel coronavirus Sars-CoV-2 can be characterised as a pandemic. The Federal Council declares a state of emergency in accordance with the Federal Law of Epidemics, shutting down non-essential businesses and services as well as closing the Swiss borders.
Shortly thereafter Gebhard Schertler, head of the Biology and Chemistry Division at PSI and professor of Structural Biology at ETH Zurich, receives an inquiry from Adriano Aguzzi. He is director of the Institute for Neuropathology at the University Hospital of Zurich (USZ) and is planning a large-scale study: He wants to use a high-throughput method to test the blood of large numbers of people in the greater Zurich area, looking for antibodies that the immune system of an infected person produces in the fight against the virus. The research project aims to shed light on how high the number of unreported cases is. "Many coronavirus infections are symptom-free, and people do not even notice that they are infected," explains Aguzzi. "So they don't take a test. An antibody study, however, will reveal the true infection rate of the population."
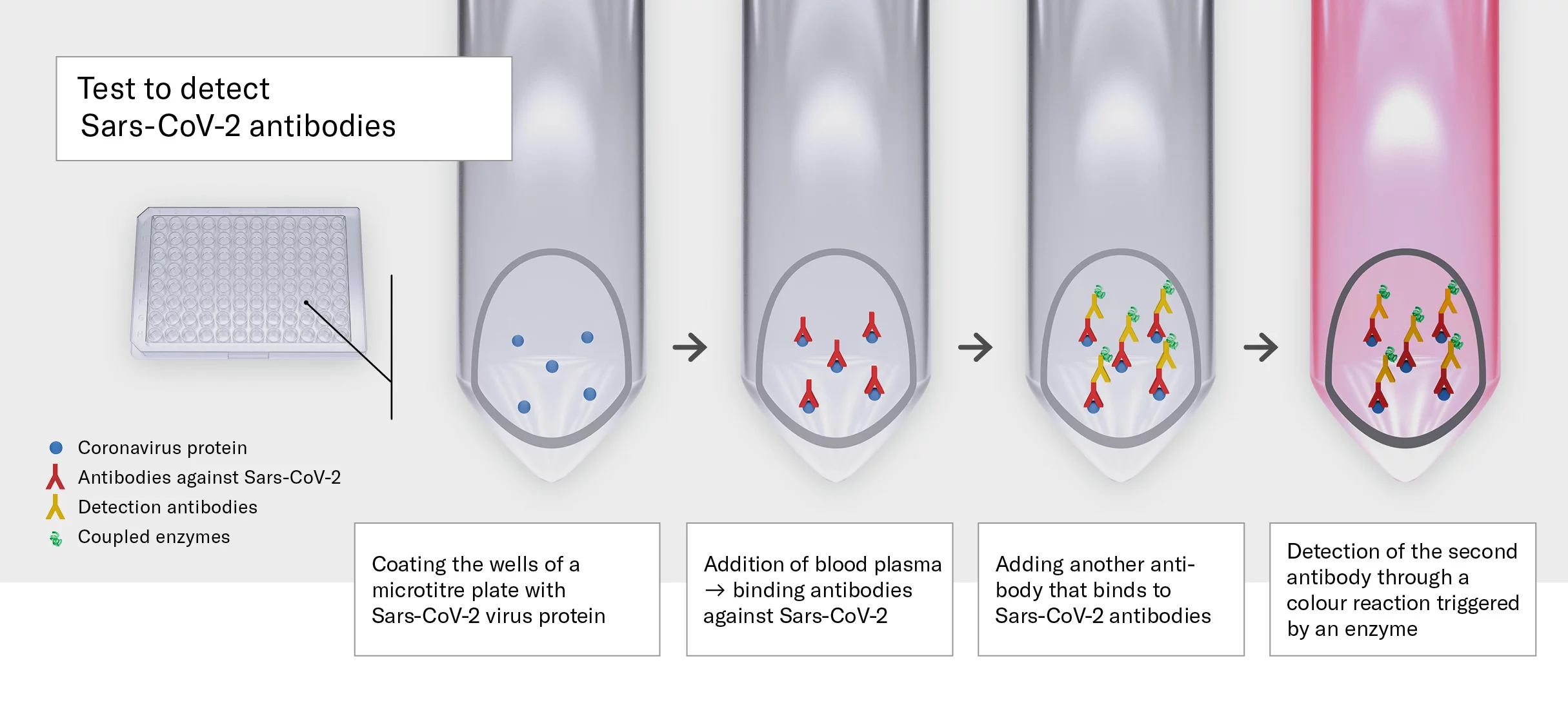
For his series of experiments, the physician urgently needs parts of the virus in a pure form: its proteins, to be precise. That's because contact with such virus proteins causes the formation of antibodies in the human immune system – large biomolecules that bind to proteins of pathogens such as Sars-CoV-2 and render them harmless. Antibodies can be detected in the blood even months after contact with the virus, and conveniently, they dock on man-made virus proteins as well as on natural ones.
Not a moment's hesitation
At that point in time, however, the coronavirus proteins are not yet commercially available in sufficient quality and quantity. So, Adriano Aguzzi turns to his large network of researchers in Switzerland and around the world, including those at PSI. "It is not at all surprising that Gebhard Schertler would be contacted in such an emergency," says Jacopo Marino, a postdoc in the PSI Laboratory of Biomolecular Research. "We've been working with very challenging proteins here for many years."
Gebhard Schertler doesn't hesitate: "We have been cooperating with the USZ for a long time, originally in the field of neurodegenerative diseases, to investigate specific proteins in the nervous system," he says. "There was no question that we would use this experience to support Adriano Aguzzi's study." Schertler asks his colleague Jacopo Marino to put together a team to produce coronavirus proteins for their peers in Zurich.
Despite the lockdown, the PSI researchers get to work immediately. In fact, no one is allowed to work in the laboratory at that time, because PSI is in the third-highest level of operational restrictions. "But we received an emergency authorisation for our work on the coronavirus," says Marino. PSI is also providing financial support for research on Covid-19.
From gene to protein
The genetic material of Sars-CoV-2 consists of a single-stranded RNA molecule that contains the blueprint for different proteins of the virus. In Aguzzi's laboratory, three of these proteins had provoked strong immune reactions in preliminary tests – in other words, after contact with them, the human body produces many antibodies that can be easily detected in blood tests. After consultation with their peers, Jacopo Marino's team decides to focus on the production of the nucleocapsid protein.
This protein forms a protective shell around the genetic material of the virus and is therefore essential for its function and reproduction. In its natural state, it forms large complexes of many molecules with the genetic material of the virus.
We literally had to become coronavirus experts within just a few weeks.
The researchers incorporate the genetic material for the nucleocapsid protein into the DNA of mammalian cells – a process that the virus also carries out when a person is infected. These cells are then allowed to grow and thrive in a nutrient solution in glass flasks for a few days. This is where they produce the protein. The next hurdle is to obtain the protein in pure form from the cell culture. PSI doctoral candidate Filip Karol Pamula ultimately develops a procedure for this.
"We literally had to become coronavirus experts within just a few weeks – like so many other research groups," says Marino. "It's good that there was already so much scientific information about other types of coronavirus."
4,000 tests in 24 hours
Within a few months, the researchers produce around five milligrams of nucleocapsid protein, freeze it in liquid nitrogen, and deliver it to the USZ. At the same time, research groups at ETH Zurich, EPFL in Lausanne, Oxford in the UK, and Yale in the USA are working at full speed to produce other protein molecules required for the study.
Adriano Aguzzi's team adds solutions of these proteins to blood samples to see if they contain antibodies against the virus. If these are detected, that means the person from whom the sample came has already been infected with the coronavirus. Since the tests are carried out with very small amounts of fluid, the physician needs correspondingly small amounts of the protein. In addition, the whole procedure is very fast: The researchers are able to perform 4,000 tests within 24 hours.
The blood samples come from completely different departments of the USZ; they had been used for examinations independent of any Covid-19 illness. The researchers also draw on blood donations – from people who should have been completely healthy at the time the blood was taken. This is a major difference from a coronavirus test based on a nasopharynx swab, which people normally have only if they are already showing symptoms – or at least have had close contact with an infected person.
Since the blood samples were taken independently of the antibody study, infection incidents can be traced back to the beginning. The researchers also measure samples from 2019 to ensure that their test does not give a positive result for antibodies against other coronaviruses, thus falsifying the result.
The second wave hits hard
After coronavirus proteins have arrived in Zurich from laboratories around the world, the team at the USZ begins the actual antibody tests. As it turns out, the number of blood samples that test positive increases slowly over the course of March 2020, reaching a maximum in April. By that point in time, according to these results, around 1.5 percent of the population in the greater Zurich area have had contact with the virus. Then the number falls back to 0.7 percent in July. Antibodies against the coronavirus can only be detected in the blood for around 100 days.
"We were all surprised that the incidence of infection in the population was so slight during the first wave," says Adriano Aguzzi. According to other studies, it was higher in other regions of Switzerland: In the canton of Geneva, for example, antibodies were detectable in almost ten percent of all people at the beginning of May. "This shows that the lockdown successfully prevented the virus from spreading across Switzerland."
Starting in November 2020, the situation looks completely different: Blood samples testing positive in the canton of Zurich reach around 6 percent in mid-December. "The second wave had a massive impact," says Aguzzi. In the canton of Geneva, however, the number is again higher at 21 percent. In general, the study shows the following: "The true incidence of coronavirus infection in the population is a good three times higher than the official tests from swabs suggest."
In the meantime, Adriano Aguzzi's team has tested over 80,000 blood samples for antibodies against the coronavirus. The study will continue for at least two years. And the promise stands: If the physician needs new supplies of nucleocapsid protein to do this, PSI will be there again to provide it.
Text: Brigitte Osterath
Further information
Copyright
PSI provides image and/or video material free of charge for media coverage of the content of the above text. Use of this material for other purposes is not permitted. This also includes the transfer of the image and video material into databases as well as sale by third parties.