In the service of people who are ill, PSI scientists work with radioactive substances and develop drugs that emit radiation. With that, they help to detect cancer and inflammation and to prevent tumours from growing. Their research provides support to hospitals and is of great interest to Swiss industry.
The race against time starts Monday morning in the clean room laboratory of the Centre for Radiopharmaceutical Sciences CRS at PSI. Doctors from the Cantonal Hospital of Baden want to examine a patient with prostate cancer and have ordered a radiopharmaceutical for the purpose, a radioactive drug. With its help, the doctors want to detect tumour cells in the patient. The agent consists of two main components. One part, the so-called tracer, precisely matches target structures that sit on the surface of tumour cells and attaches itself there. The second component signals the location through radioactivity. It consists of a radionuclide. This term refers to unstable atoms that emit radiation as they decay. For medicinal purposes, radionuclides with a half-life of a few minutes to a week are employed. Because of the radioactivity, their production is only allowed under certain safety measures, which are provided at PSI. For prostate cancer diagnostics, the team in the clean room laboratory produces the radioactive drug 68Ga-PSMA-11. That requires two days of preparation, but Wednesday, on the production day, there is a big rush in the lab – in just 68 minutes, the particular radionuclide being used loses half of its radiation intensity.
- 10:00: In a so-called hot cell shielded with thick lead plates, the synthesis of the active agent starts at the push of a button. Slowly, a nondescript, clear liquid drips from the synthesis apparatus into a vessel.
- 10:40: The liquid with the agent is transferred to a thumb-sized glass bottle and packed in a radiation-safe container.
- 11:00: The drug is ready for transport by a dangerous-goods carrier. The container will arrive at the hospital 30 minutes later. The patient is already waiting there.
- 11:30: The team at PSI checks a retained sample of the drug for quality and purity and informs the clinic of its approval.
- 12:00: The specialist draws the quantity of the active agent calculated for this patient into a syringe and injects it into the patients veins. The examination is under way.
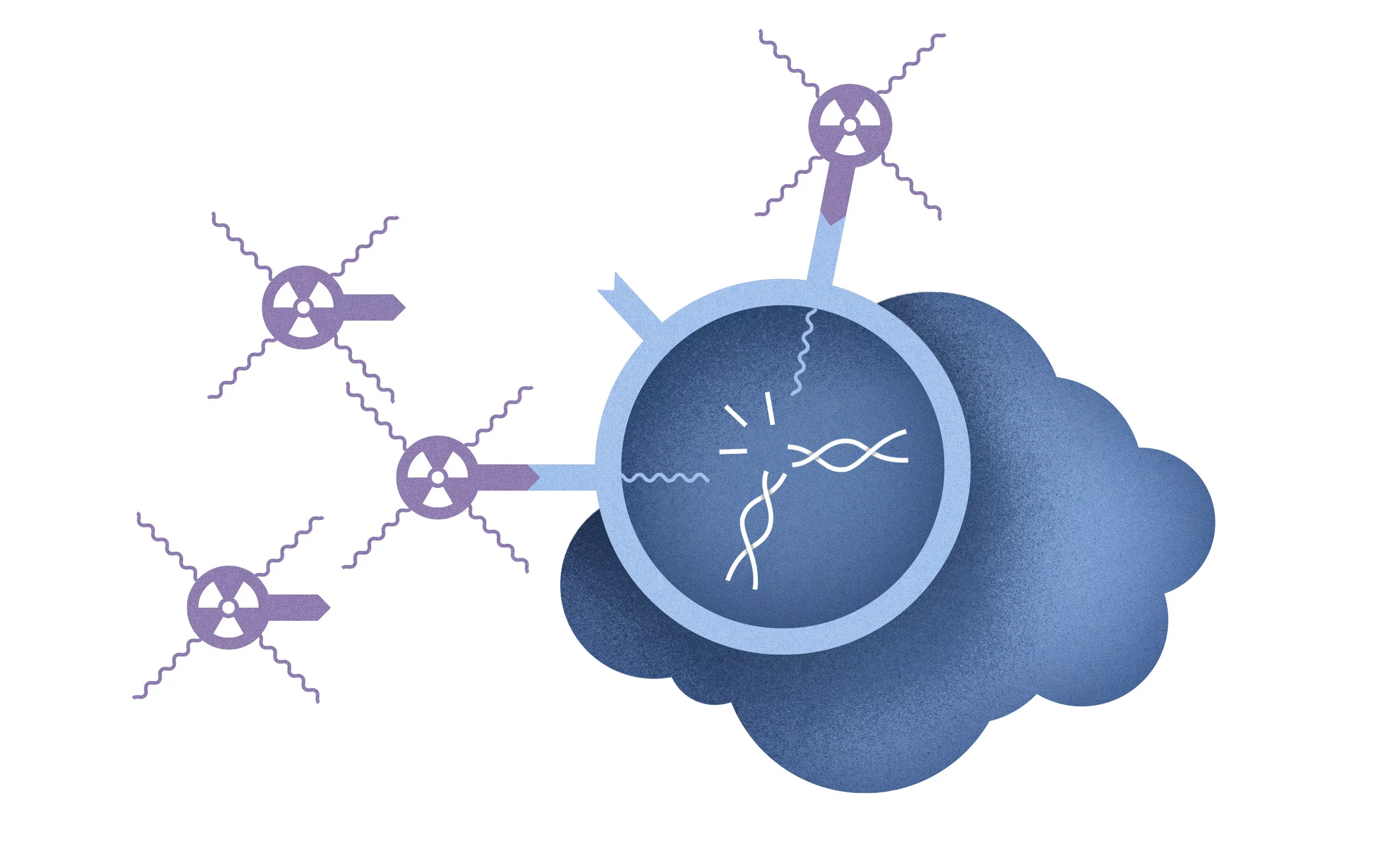
Once it is in the blood stream, the radioactive drug seeks out its target in the body: the cancer cells. These carry on their surface structures that are characteristic of a particular type of cancer and that healthy cells do not exhibit. The drug coupled to the radionuclide docks on these structures.
The radiation emitted by the drug makes tiny fragments of the tumour visible, which otherwise could not be seen. This is accomplished with the help of special cameras. They capture the radiation that the agent sends out from the patient's body. From that, a computer calculates images on which the tumour sites appear in colour and are easily recognisable. On this day, too, the agent used fulfills its task, and the doctors of the Cantonal Hospital of Baden now know where the tumour and its offshoots are located in the patient's body. This information is used to develop a therapy tailored to the patient's situation.
But radioactive substances can do much more than track down cancer cells. "The properties of a radionuclide determine whether it will be used for diagnostics or to selectively destroy the cancer cells", explains Roger Schibli, head of the CRS, a joint institution of PSI, ETH Zurich, and the University Hospital of Zurich. Some radionuclides, such as lutetium-177, also emit destructive particle radiation, so-called beta radiation, which only travels a few millimetres. It can directly destroy cancer cells as soon as the radiopharmaceutical docks on them.
Martin Béhé and his research group at CRS exploited the special radiation characteristics of lutetium-177 and coupled the radionuclide to a minigastrin tracer. This molecule selectively binds itself to the so-called cholecystokinin-2 (CCK2) receptor, which tumour cells of the malignant thyroid carcinoma carry on their surface. In this type of thyroid cancer, the otherwise well established radioiodine therapy is not effective. This cancer quickly forms metasteses in other organs and often affects children and young adults. "Once this tumour has formed metastases, a cure has not, up to now, been possible", Béhé says. Therefore, he and his team searched several years for a radioactive agent to find and destroy the metastases. The researchers intensively investigated what agent is rapidly absorbed in the body, binds only to the CCK2 receptor, and quickly leaves other tissues so that its radiation will not harm healthy cells.
These and other special requirements made the search for a suitable substance difficult. The researchers did not succeed until they combined the peptide minigastrin (PSIG-2) with lutetium-177: It accumulated selectively on the cells of the medullary thyroid cancer, did not remain in other tissues, and was rapidly excreted from the kidneys, so that no damage would be done there. With that, the most important prerequisites were met to move on to production of the agent, according to standards mandated by pharmaceutical regulations, in the clean room laboratory at PSI – the first step towards monitored use in patients within the framework of a study. In 2016, the time had finally come: With the permission of the drug approval and supervisory authority Swissmedic, doctors at the Clinic for Radiology and Nuclear Medicine of the University Hospital of Basel were allowed to treat patients for the first time with the new agent, which in the meantime had been patented. "In this first study, we gave the agent to six patients with an advanced stage of medullary thyroid cancer", reports Christof Rottenburger, a Basel-based physician who specialises in nuclear medicine.
The properties of a radionuclide determine whether it will be used for diagnostics or to selectively destroy the cancer cells.
At this time, PSI published information on its website about the development of the agent and its approval as a study drug. This article aroused the interest of the Swiss pharmaceutical industry. The Lausanne-based company Debiopharm contacted Martin Béhé at PSI. The businesspeople learned about the composition of the agent and how it was produced in the PSI laboratory, posed questions and reviewed documents, and took a close look at the results of the first patient study. The result was convincing: In December 2017, Debiopharm and PSI signed a licencing agreement that allowed the company to further develop the PSI drug for applications in cancer treatment and bring it to the point of approval and thus market-readiness. In July 2018, the time had finally come: The agent, called 177Lu-PSIG-2, is now also named after the Lausanne-based pharmaceutical company: Debio1124.
Meanwhile, at the University Hospital of Basel, the second part of the patient study with the PSI agent has begun. "This study is a so-called dose-escalation study", Rottenburger eplains. "Here we give patients with medullary thyroid cancer a dose of the agent that is considered safe and observe whether they tolerate this dose well and without serious side-effects on other organs. If this is the case, then the dose of the agent can be further increased." With this approach, the physicians in Basel work together with PSI to determine the radiation dose patients can safely receive for treatment. For the duration of the study, the radioactive drug will continue to be produced in the clean room at PSI – along with other radiopharmaceuticals ordered by the clinics in the region. At the CRS, researchers are already working on the next promising substances.
Text: Sabine Goldhahn
Further information
This is how radionuclides are produced at PSI: In the focus of the protons