Interview with Damien Charles Weber
Protons have been used to treat cancer patients at today’s Paul Scherrer Institute since 1984. For certain types of tumour, the method enables a particularly targeted approach, where the tumour tissue is combatted successfully and the surrounding tissue optimally preserved. The treatment of ocular tumours just goes to show how successful proton therapy has been: in 98 per cent of all cases, tumour growth was halted definitively.
Damien Charles Weber has been Head of the Centre for Proton Therapy at PSI since 2013 and also holds chairs at the Universities of Zurich and Bern. In the following interview, he explains what it means to run a medical treatment centre at a research institute. He mentions that, in the foreseeable future, proton therapy might also to be used to treat tumours in moving areas, such as the upper abdomen or around the lungs. Moreover, the expansion of the centre is also in the pipeline: supported by the Canton of Zurich, an additional area for cancer treatment is to be established in 2016.
Mr Weber, has the use of proton therapy to treat tumours been a success story at the Paul Scherrer Institute?
Definitively! When ocular tumours were first irradiated with protons here in Villigen in 1984, PSI had the first facility in Europe. In the last twenty-five years, over 7,000 patients have been treated here. 98 per cent of our eye patients are considered locally controlled. Moreover, we've treated over 1,000 patients with tumours deep in the body at our treatment units Gantry 1
and Gantry 2
, where we have also had very encouraging results with a tumour control rate of more than 70–80 per cent for certain tumour entities.
A large number of children suffering from cancer are treated at PSI. What makes proton therapy so important for this particular patient group?
Children are smaller than adults and their organs are located a lot closer together in the direct vicinity of the tumour volume, which makes it difficult to irradiate the tumour tissue without affecting other organs as well. With conventional radiotherapy, the radiation doses can be controlled less precisely and also have a wider scattering than irradiation with protons, which unleash their destructive effect very precisely on the points calculated in the cancerous tissue and not the healthy tissue.
As Chairman, you run a medical centre at a research institute. Do you sometimes feel a bit like a rare breed?
Yes and no. This dual role has advantages for PSI's team and the patients. On the one hand, patients are treated highly successfully at the Centre for Proton Therapy. On the other hand, we keep driving the research forward. Techniques are developed here that won't be implemented for another five to ten years in other centres. We benefit from the interaction between medical physics and beam therapy in this respect. It always triggers exciting discussions as people with completely different backgrounds are looking for the best possible solution for a given case.
What makes the work at the Centre for Proton Therapy so appealing for you?
The 5 or 6 per cent of cancer patients who are treated with radiotherapy and cannot be treated with conventional radiotherapy. We look for the best strategy for every one of these special cancer cases, which are rarely seen in busy radiotherapy departments.
What brought you to PSI?
I'd already worked here at PSI's Centre for Proton Therapy in 2003/04 so I knew the field and the environment. When the opportunity came up to take over the helm in 2013, I couldn't resist the challenge.
What are your goals for the next few years?
Like everywhere, everything is starting to age in our proton therapy centre. Our equipment and the software were all developed in-house at PSI in the 1990s. At the time, it was pioneering and it's still among the best in the field today. But you can't ignore the fact that it is becoming increasingly harder to maintain and keep it in working order. We need to modernise these systems, integrate them in a modern IT infrastructure and partly switch to technologies available on the market. This is particularly true for our treatment planning system.
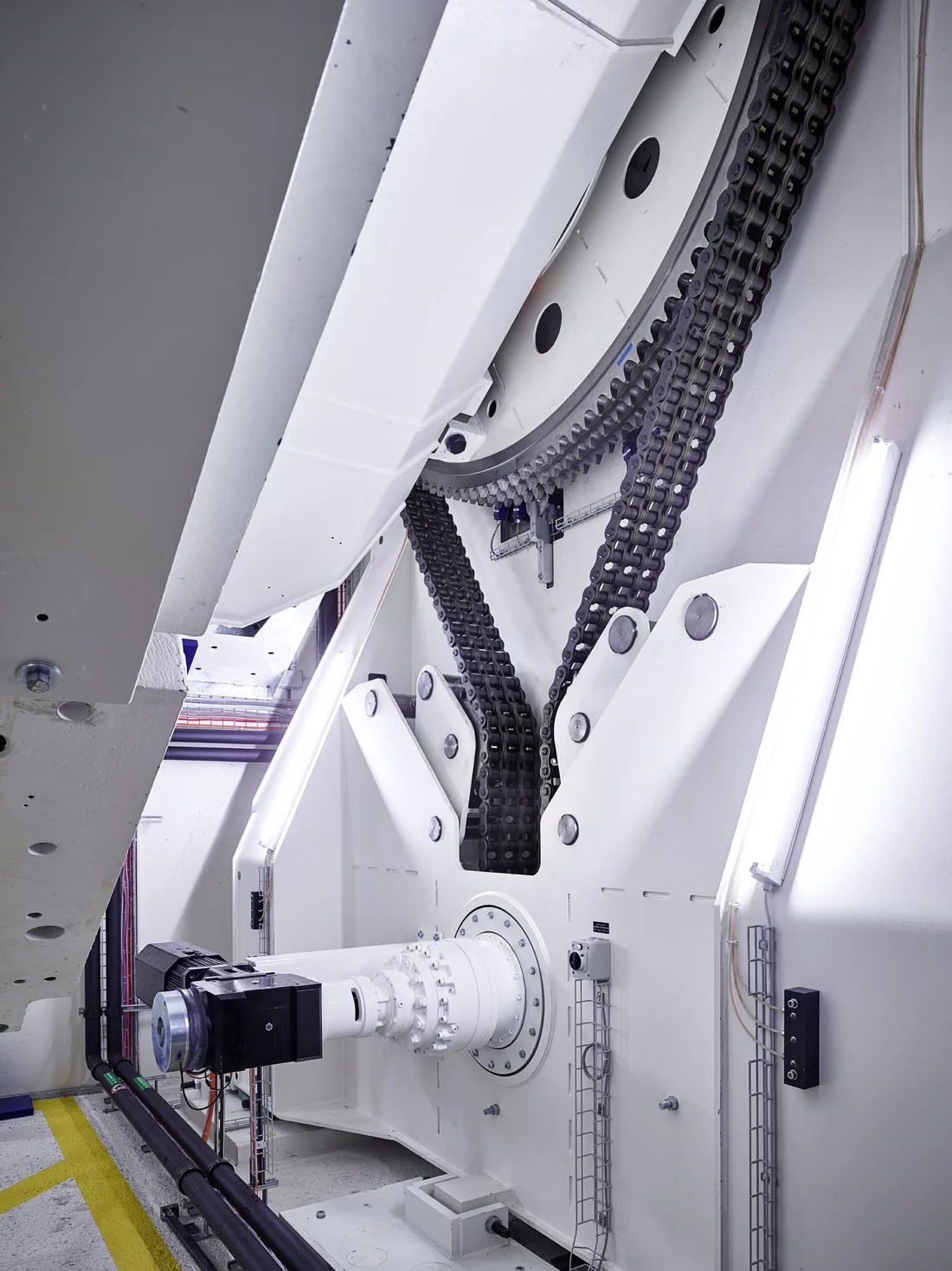
Is the treatment station Gantry 3
one such case, where you're buying on the market as opposed to developing it yourselves?
If we had to build Gantry 3
ourselves, it would take far too long. As the Canton of Zurich is putting up CHF 20 million from the lottery fund for this project, it wants to get started with treating patients soon. Consequently, the treatment station is initially being designed in collaboration with a commercial developer of this kind of equipment, bearing in mind that all the challenging specifications have been defined by PSI.
Where will the path in proton treatment lead in years to come?
In future, we also want to be able to treat tumours that inevitably move during respiration on account of their position in the upper abdomen or in the lung. This means that the proton beam needs to be able to follow these movements precisely. We may well reach this stage in a year's time.
And what's the next step for the development of proton therapy?
We are developing an even more appropriate scanning paradigm, which we refer to as the repainting strategy
. We repeatedly paint
over the tumour with tiny quantities of radiation.
Ambitious plans. You don't just work at PSI but also hold chairs at the Universities of Bern and Zurich. How do you find the time for it all?
I've got a clinical project on the go on a 10-per-cent basis at the University Hospital of Bern. I also work 10 per cent in Zurich. You have to be extremely well organised and have an excellent team. I was also lucky enough to have a great assistant, who takes a lot of the load off. I try to foster frequent contact with my staff in unconventional ways as I'm not on site 100 per cent of the time. If there's time, we go for a coffee or lunch/dinner to exchange the soft information.
Interview: Alexandra von Ascheraden
About the person
Born in French-speaking Switzerland, Damien Charles Weber has been the head and chief physician of the Centre for Proton Therapy (ZPT) at PSI since September 2013. He is a professor of radio-oncology at the Universities of Zurich and Bern. After completing his degree in medicine in Geneva and his specialist exam in oncology/radio-oncology, Weber worked at Harvard Laboratory Cyclotron and at North East Proton Therapy Center in the US in the field of proton therapy. Upon his return from the United States, he worked at PSI and in Geneva again as a deputy chief physician. Weber is also President of the Scientific Association of Swiss Radiation Oncology. His wife is a doctor specialising in medicine for children and young people. The couple has two grown-up children. In his spare time, Weber likes to go sailing and skiing.Proton therapy at PSI
PSI runs Switzerland's only centre for proton therapy. It contains a treatment unit for ocular tumours called OPTIS. Moreover, the therapeutic centre has two irradiation units -Gantry 1and
Gantry 2- for the treatment of deep-seated tumours. A third gantry is currently under construction, which should be available for use on patients from 2016. Unlike the irradiation techniques otherwise used in radiology, protons spare the surrounding healthy tissue but still successfully prevent the tumour from growing. Using the spot-scanning technique developed at PSI, deep-seated malignant tumours can be irradiated with pinpoint precision. The method is only suitable for certain tumour diseases. A list is available at www.psi.ch/protontherapy/indications.