Protons can accurately target and eliminate cancerous cells by erasing their genetic substance DNA. Doctors at the Centre for Proton Therapy at the Paul Scherrer Institute PSI use protons to treat patients with deep-seated tumours or ocular cancer. In order to make sure that proton beams hit only the targeted cells and do not damage healthy tissue, a large number of safety measures are in place every time a patient undergoes irradiation. It's essential that these measures work accurately—which is why an extensive team of specialists devotes itself to patient safety every day.
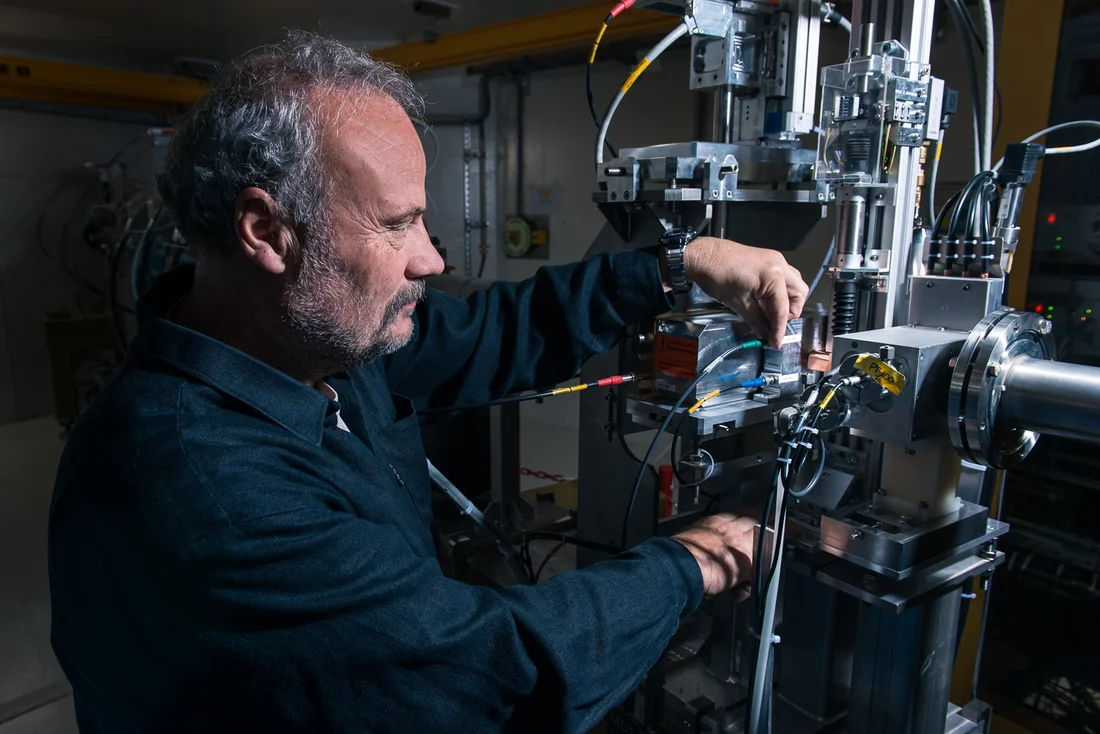
It's six o'clock in the morning and all is quiet in the dimly lit rooms at the Centre for Proton Therapy CPT. There are no patients in the waiting room, the reception area is empty and in the treatment rooms, the high tech facilities are on stand-by mode. They look like sleeping giants. No employees to be seen. Only the on-duty technician is ready to begin the day by pressing the buttons that activate the three treatment units for proton therapy at the Paul Scherrer Institute: Gantry 1 and 2 as well as OPTIS. The computers start up with a low hum and the numerous screens in the control rooms start to flicker. Each of the three units is subjected to a twenty-minute safety test based on strict, standardized guidelines and subsequently counterchecked and signed off by two specialists. It takes two hours to complete the whole procedure, make sure that the units are working correctly, and iron out any faults. Only then, after 8 o'clock, are the first patients admitted for proton irradiation.
Over 350 Safety Tests a Year
We have a total of 43 procedures that need to be checked every morning and more than 300 more that require checking once a week, once a month or twice a year
, says Gerhard Aigner, responsible for safety and quality management at the CPT. The walls in his office are lined with user manuals, safety instructions and signed test protocols. Aigner needs to know when such tests are necessary to maintain the installation's safety and to make sure that they've actually taken place. Just carrying out our routine morning check involves simple measures such as testing the audio equipment that patients use to talk to operators as well as complex physical tests involving the so-called Daily-check-Phantom.
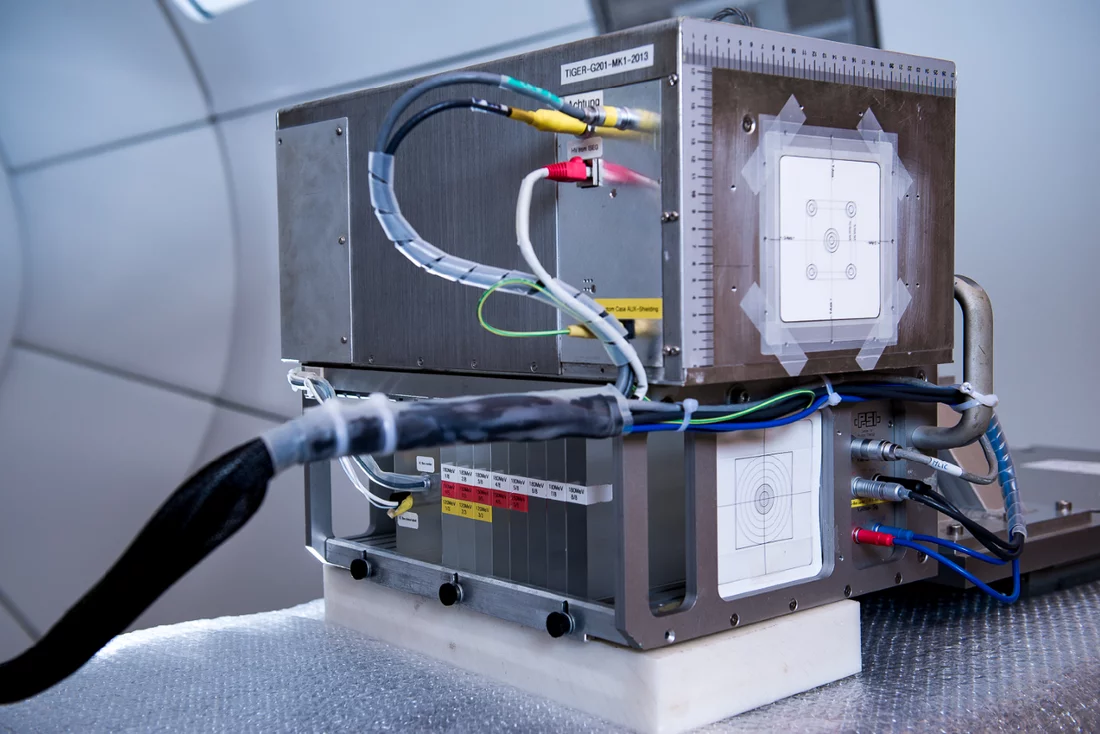
This is the name given to a large white box, stuffed to the brim with electronics. Every morning, a technician places the box in the proton beam path emanating from each of the three units—right where the patient normally receives treatment. The beam is loaded with specific radiation dosages and directed at pre-determined points on the phantom to make sure that the beam's dosage and target accuracy are correct.
Protons have a high degree of precision, making it possible to treat inaccessible or sensitive points in the body with an accuracy that diverges by less than one tenth of a millimetre from it's target
, explains physicist Martin Grossmann from the CPT. But this advantage can only be used if the patient is correctly positioned in the beam path, on either the treatment chair or couch. So far, we have succeeded in achieving a precision of about one millimetre.
The precise positioning of patients undergoing treatment in the three units is determined by specific computer programmes, which Grossman and his team developed years ago. A particular challenge consists in situating the patient in exactly the same position over several weeks of treatment. This is why every proton irradiation session involves an x-ray on which anatomical markers control the patient's correct position.
Better than Industrial Standards
But what happens when the beam itself goes off course? In such cases, a whole battery of emergency measures kicks in to ensure that the protons don't target the wrong spot. Grossmann and his team are especially proud of the way these measures have been developed, programmed and implemented: When we pioneered the spot-scanning technique in our first Gantry twenty years ago, we wanted to be absolutely sure that this new form of proton irradiation stayed accident free when used on patients. Since there were no official regulations in place, we incorporated five safety barriers—more than the number required today for commercial providers. Without the cumulative knowledge of the specialists working here at PSI, this wouldn't have been possible.
Those five safety barriers still exist today and are programmed to become active one after the other. If one doesn't work, the next one starts up.
Doctors and medical physics staff develop individual treatment plans for each patient specifying the exact location of the tumour on a virtual three dimensional system of coordinates as well as the irradiation dosage and duration for each individual spot in the tumour. This treatment plan is stored in the computer and steers the automatic piloting system in both two-ton irradiation units Gantry 1 and Gantry 2. Every irradiation is subject to safety objectives: the dosage must tally with the plan to within one per cent, and the beam position must be calculated to hit each spot in the tumour at all three levels with maximum accuracy, allowing only for an error margin of 1 millimetre. Various gauges register the beam path for the duration of each irradiation to ensure that these guidelines are observed. Whenever this is not the case, the beam is automatically turned off: after a latency period of less than one millisecond, the first safety element kicks in.
Thirty Accident Free Years
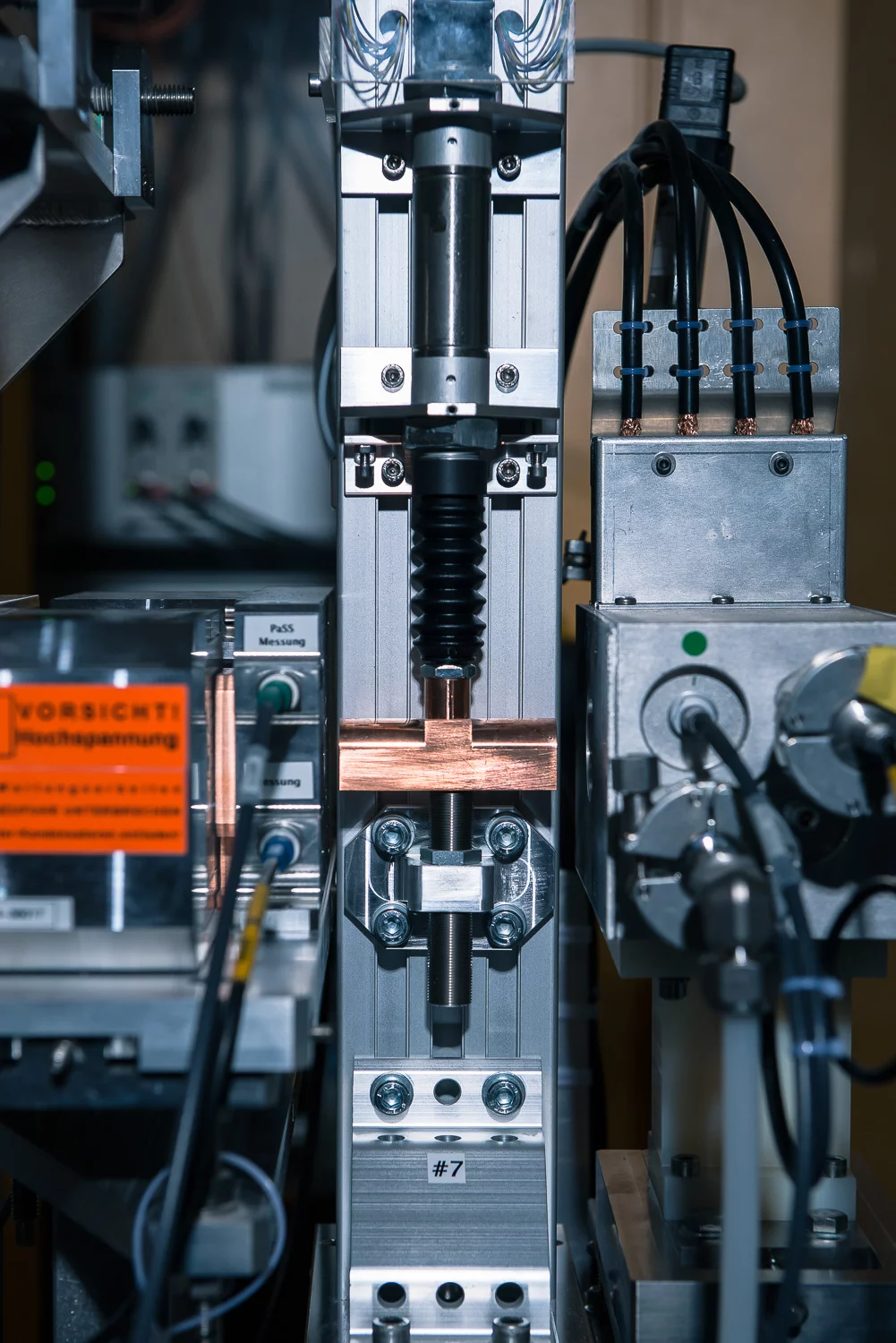
Inserting blocking systems such as a five-centimetre-thick copper block into the beam stops the protons and prevents them from reaching the patient
, explains Grossmann. The first two blocking systems shoot the copper block into the beam using compressed air, which makes them especially fast. In case both these systems fail, the third system—which works with gravity and uses a steel blocker—starts up. Situated at a distance of about fifty metres, the accelerator that propels the proton beam at sixty percent the speed of light shuts down even more quickly. The last of the five safety barriers is located directly at the source of the proton beam, near the gas cylinder filled with hydrogen that delivers the protons. Grossmann, who has been on board for twenty years and knows every nut and bolt in the units, sums up the situation: Currently, we can look back on thirty accident free years
, he says, during which we've treated several thousand patients.
Staff at the CPT excel at implementing the high safety standards in place at all three proton therapy units, all of which were developed at PSI. This year, the fourth unit, a new Gantry, will go into operation. Gantry 3 represents a new departure for the CPT since it is the first unit acquired from a commercial provider. In theory, that should have made things work more easily, requiring only one push of a button. But as far as Gantry 3 was concerned, the challenge for Grossmann's team lay elsewhere. The new irradiation apparatus had to be connected and adapted to PSI's own accelerator. The physicist emphasises that constructing this interface required some considerable effort on the part of the PSI team. The most difficult task was reconciling the different approaches to beam steering, overall control and safety measures.
Based on common practice, the provider had only incorporated two safety systems. PSI has five. So the specialists started working on ways of applying the five safety systems when the new unit was in use. Gantry 3 should be ready to treat its first patients at the end of this year, after which the physicists and technicians at the CPT can turn their attention to other challenges again.
Working into the Night
One of the challenges they face is reducing the duration of irradiation treatments in Gantry 2 and treating patients even more quickly. They aim to achieve this by moving the proton beam continuously over the tumour, like a pencil drawing a line on a piece of paper. The spot-scanning technique for treating a tumour can be compared to a pencil placing many dots next to one another. Every time a new dot is made, the proton beam is briefly interrupted before moving on to the next. This takes time. The first stages necessary for the development of this new technology have been completed. The next step will be to programme and test new safety systems for this procedure. These and other research projects as well as the calibrations and measurements necessary for quality management tend to take place in the evenings and during the night. When the patients have gone home and it starts to get dark outside, staff at the CPT start exploring new territories.
Text: Sabine Goldhahn
Further Information
- The article Big help for small children describes how children suffering from cancer are treated with proton therapy at PSI’s center for proton therapy.
- For an overview of the work carried out at the Centre for Proton Therapy (CPT) and the development of proton therapy at the PSI see the article Added value for cancer patients.
- A special form of proton therapy called spot-scanning technology was developed over twenty years ago at the PSI. This method is now used worldwide and has already helped several thousand patients. Details are provided in the article entitled 20 Years of high-precision combat against cancer.
- Proton therapy at the PSI started with the irradiation of ocular tumours. To date, the PSI itself has treated 6,700 patients. For more information, please see the article Rays of hope for patients.
Contact
Dr. Martin Grossmann Handschin, Physicist at the Centre for Proton TherapyPaul Scherrer Institute, 5232 Villigen, Switzerland
Telephone: +41 56 310 36 33, e-mail: martin.grossmann@psi.ch
Gerhard Aigner, Office of Safety and Quality Management
Centre for Proton Therapy
Paul Scherrer Institute, 5232 Villigen, Switzerland
Telephone: +41 56 310 34 48, e-mail: gerhard.aigner@psi.ch
Dr. Ulrike Kliebsch, Responsible for Science and Information Services at the Centre for Proton Therapy
Paul Scherrer Institute, 5232 Villigen, Switzerland
Telephone: +41 56 310 55 82, e-mail: ulrike.kliebsch@psi.ch