Tumours of the eye are rare. Yet for those affected, they mean a stroke of fate that involves not only the loss of vision but often the whole eye as well. That is why, for more than 30 years, an entire team at the Paul Scherrer Institute PSI has been dedicated to helping patients with a particular form of ocular tumour — by means of proton irradiation. The tiny particles hit their target with millimetre precision without endangering other structures of the eye. At no other proton therapy facility in the world have so many patients with ocular tumours been treated, as at the OPTIS facility developed here at the Center for Proton Therapy at the Paul Scherrer Institute PSI. OPTIS is a success story, because for more than 90 percent of the patients treated to date, the eye could be saved.
The eyes are our window to the outside world and one of the most important sensory organs. They capture visible information from our surroundings and transmit it to the brain, which processes it. This allows us to see what is around us and experience the world in three dimensions. At the same time, we communicate with other people through eye contact and express our feelings with our eyes. When one eye is attacked by cancer, the person affected often doesn’t notice it at all, because the brain still receives information from the healthy eye and compensates for the loss. A hazy area, a small flaw in vision, is sometimes the only thing one notices. Thus many ocular tumours are found accidentally in the course of a routine checkup by an eye doctor. One particularly malignant form of ocular tumour has been very successfully treated for years at the Paul Scherrer Institute PSI: ocular melanoma. It is related to the skin cancer known as black cancer
and likewise originates in pigmented cells. Such cells are found primarily in the choroid, a vascular layer between the inner retina and the outwardly visible white dermis.
Ocular melanomas are sometimes only one to two millimetres in size, and even so they can give rise to metastases through the bloodstream, mainly in the liver
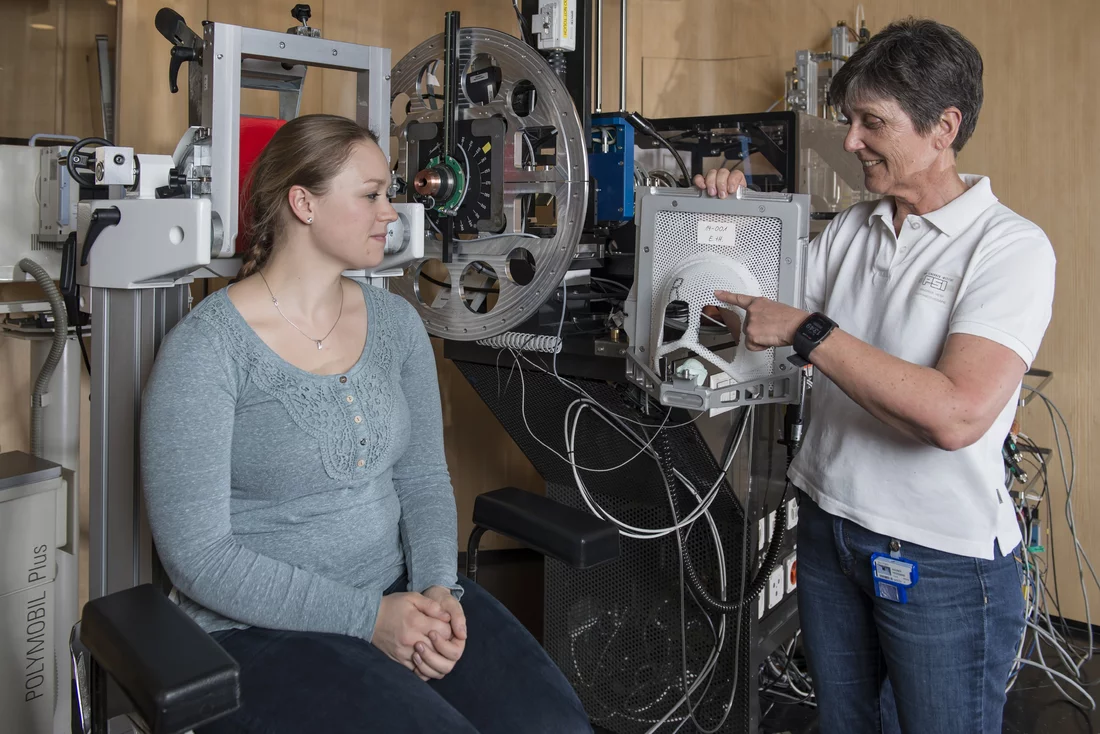
, explains Heidemarie Wagner, a radiation therapist at the Center for Proton Therapy CPT of PSI. That’s why early treatment is so important.
The experienced radiation therapist knows exactly what she’s talking about, since she has been working here for 12 years at the irradiation facility OPTIS, where exclusively ocular tumours are treated. Heidemarie Wagner is proud of her workplace: More than one-third of all patients in the world who have received proton irradiation for ocular tumours were treated here at OPTIS — 6,700 patients. And the beautiful thing is that, in 90 percent of all cases, we have been able to preserve the eye while destroying the tumour.
In all those years, she has prepared several thousand patients for the irradiation treatment, explained everything to them, comforted them, and tried to ease their fear. When the patients are referred to us, they already endured many examinations and an operation at the university eye clinic in Lausanne
, Wagner says, which can be demoralising.
Metal clips for irradiation planning
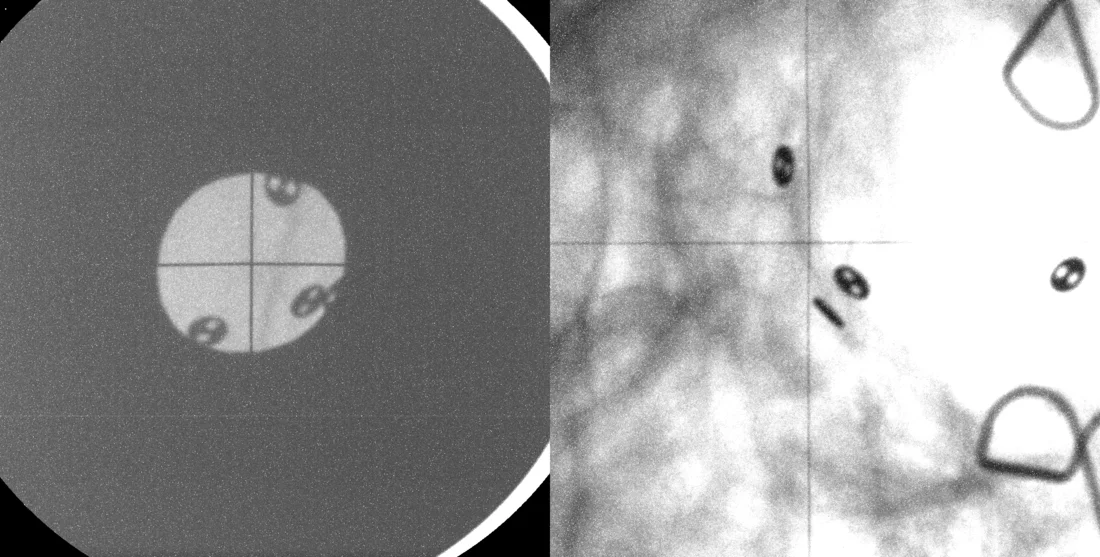
Lausanne is the coordination site for the treatment of patients with ocular tumours. Patients are referred there from many European countries to prepare them for proton irradiation at the CPT. First, eye doctors in Lausanne must mark the tumour so that the CPT specialists can later localise it as target for the proton beam. Coming from the back side of the eyeball while the patient is under anaesthesia, the eye doctors attach four to six tiny metal clips made of tantalum around the tumour . Medical physicist Jan Hrbacek of the CPT explains why: These metal clips appear on X-ray images as black, button-like dots. Thus we can use them as markers to help us locate the tumour and isolate it. The tumour itself cannot be seen in X-ray images.
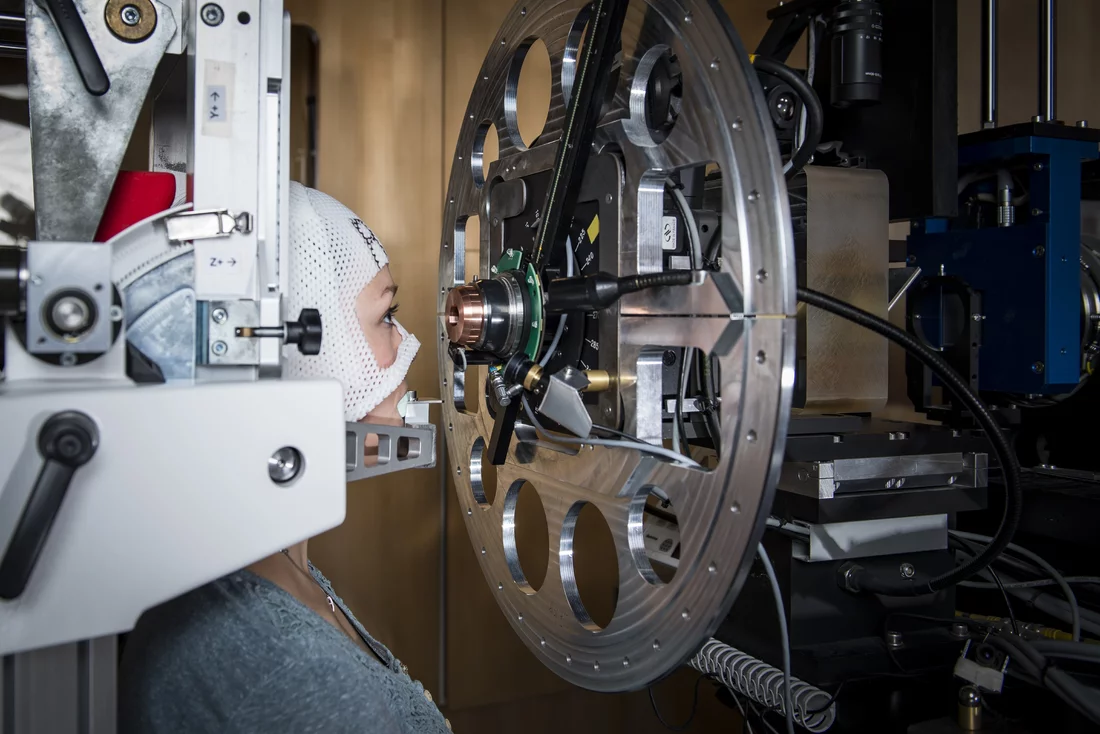
Much preparation is necessary in order to let Hrbacek know exactly where he needs to direct the proton beam. Most importantly, during treatment, the patient must hold the head perfectly still, because he or she is sitting right in front of the beam of superfast protons. Even a light twitch would be enough, and the proton beam would hit the wrong place. To avoid this, a mask is custom made to fit the patient before treatment begins and a bite block — that is, a cast that fits the patient’s teeth, to bite down on during irradiation. These two components are fastened to the mask frame and thus permit no head movement. Only the eyes can still move. During irradiation, the patient must always actively work with us
, Wagner emphasises, because the proton beam always comes from the same direction, from directly in front of the patient
. Therefore, the patient has to turn the eye so that the tumour is exactly in the path of the proton beam. But how does the patient know where to look?
Eye contact with OPTIS
As a basis for each irradiation, the medical physicists at CPT use special software to construct a three-dimensional virtual model of the eye and the tumour. They first feed patient-specific information into the model, such as the length of the eyeball and the thickness of the lens, as well as the exact distances between the individual metal clips and between the clips and the tumour. When the patient comes to PSI for the first time, the radiation therapist takes two X-ray images of the head from different directions. These show only the bony structures of the eye socket and the metal clips, which lie in a specific pattern relative to each other. When the patient moves the eye, and with it the tumour, the position of the metal clips in the X-ray image also changes. Using the model, Hrbacek and his colleagues then calculate which viewing direction is best suited to ensure that the proton beam will hit the whole tumour and leave out sensitive structures like the optic nerve, the lens, and the cornea. The patient must look in this direction, which is indicated by a small LED light on the device. When we know what the optimal eye position is, we also know the optimal position of the clips
, Hrbacek says. These must match each other absolutely at every irradiation session. Before treatment, therefore, control X-rays are taken which depict the metal clips.. A 0.2-millimetre deviation is still permissible
, Hrbacek says, and then it is corrected
.
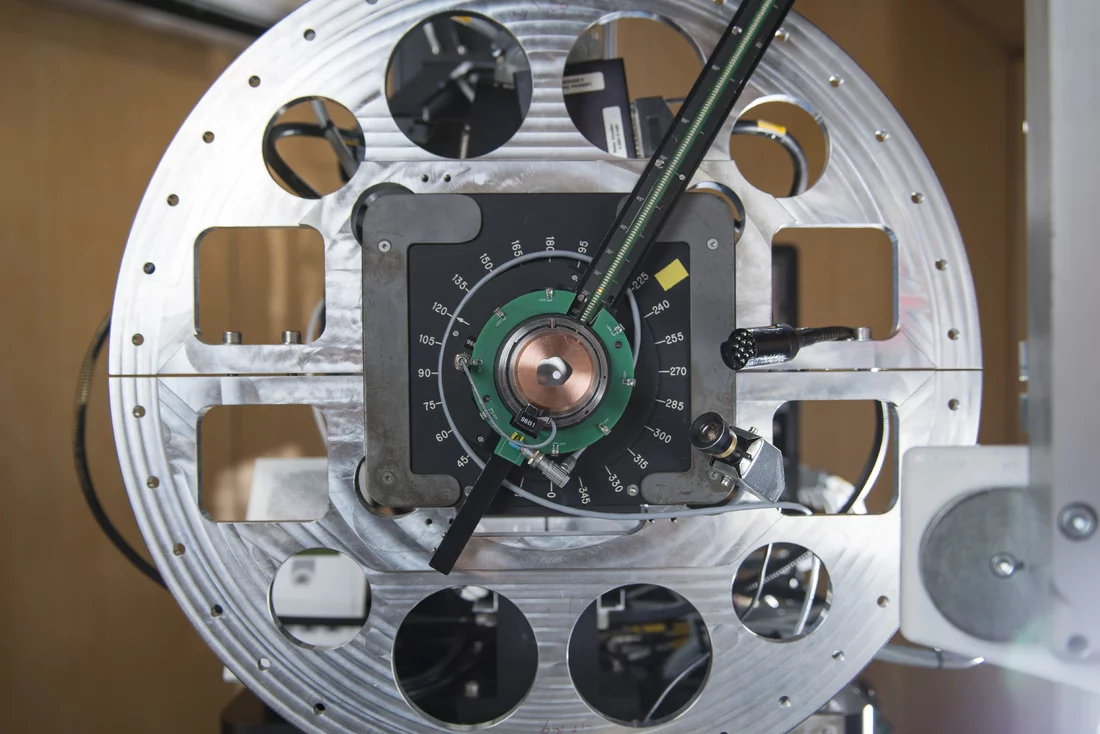
Focused on the tumour
Protons destroy the genetic material DNA, so that the cells can no longer divide or grow. To successfully kill off all cancer cells in the eye, the beam must cover the full extent of the tumour. To that end, the proton beam is confined to the specific shape and size of the tumour by a type of aperture plate. At the same time, as far as possible, healthy tissue should be spared. Here, a particular characteristic of the proton beam proves advantageous. It is a property that distinguishes it from other types of irradiation: The beam exerts its maximum effect at a predetermined depth. This depth is set on the OPTIS device. Cells that lie before or behind the target site are not damaged by the protons. Normally, four irradiation sessions on directly consecutive days are sufficient, and then the treatment is finished. Heidemarie Wagner: Our patients are generally in a good state of health, and they are still fine after irradiation because they have no side-effects. So they can go right back to their normal life.
Future plans for OPTIS Proton irradiation of ocular tumours at PSI is a success story. The specialists at CPT could rest on their laurels, if not for one thing that disturbs engaged researchers like Jan Hrbacek: Up to now, every patient has to undergo an operation under anaesthesia for the implantation of the metal clips. We would like to avoid this.
His goal is a model of the eye that would make clips completely unnecessary for positioning. In a project funded by the Swiss National Science Foundation and approved by the Ethics Committee, he is using magnetic resonance imaging (MRI) to test how to best integrate high-resolution images of ocular tumours into a new virtual eye and tumour model. The model is complemented by an optical tracking system that captures the position of the eye in the OPTIS device and thus aids in localisation. Only when the new method functions accurately and with complete reliability will the patients be spared the surgical intervention. The researchers at PSI are working toward this goal.
Text: Sabine Goldhahn
Additional information
- The article Big help for small children describes how children suffering from cancer are treated with proton therapy at PSI’s center for proton therapy.
- For an overview of the work carried out at the Centre for Proton Therapy (CPT) and the development of proton therapy at the PSI see the article Added value for cancer patients.
- A special form of proton therapy called spot-scanning technology was developed over twenty years ago at the PSI. This method is now used worldwide and has already helped several thousand patients. Details are provided in the article entitled 20 Years of high-precision combat against cancer.
- A whole team of specialists is responsible for proton therapy safety and quality standards at the PSI. For details please see Getting a handle on safety.
Contact
Dr. Ulrike KliebschResponsible for Science and Information at the Center for Proton Therapy
Paul Scherrer Institute, 5232 Villigen PSI, Switzerland
Telephone: +41 56 310 55 82, e-mail: ulrike.kliebsch@psi.ch
Dr. Jan Hrbacek Medical physicist
Center for Proton Therapy
Paul Scherrer Institute, 5232 Villigen PSI, Switzerland
Telephone: +41 56 310 37 36, e-mail: jan.hrbacek@psi.ch
Heidemarie Wagner Radiation therapist Center for Proton Therapy
Paul Scherrer Institute, 5232 Villigen PSI, Switzerland
Telephone: +41 56 310 54 13, e-mail: heidi.wagner@psi.ch