Developed at the Paul Scherrer Institute PSI, the spot-scanning technique for proton therapy has been treating patients, gently and efficiently, since 1996.
At the Paul Scherrer Institute PSI on the 25th of November, 1996, the first cancer patient worldwide was treated with a new irradiation method: the so-called spot-scanning technique for proton beams. With this technique, a thin proton beam scans across tumours inside the body and destroys them. What’s special about it: The beam has its effect only at the depth where the tumour is located; healthy tissue above and below it is preserved. The method developed by the PSI researchers was a breakthrough at the time and quickly became a successful product: Today spot scanning is the standard method in proton therapy and is used worldwide in dozens of specialised centers. Already, more than 1200 cancer patients have been routinely treated with it at the Center for Proton Therapy of the PSI.
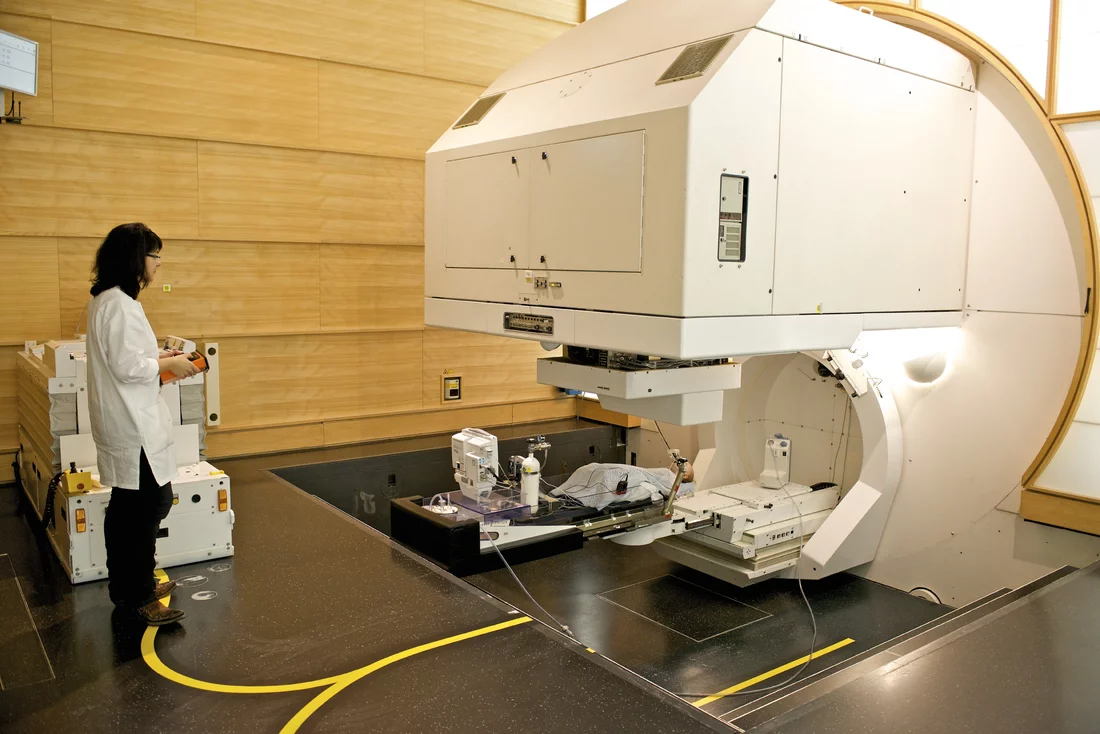
At the Paul Scherrer Institute PSI 20 years ago, on 25.11.1996, the then brand new spot-scanning technique in proton therapy was applied for the first time worldwide to treat a patient. With wintry cold weather outside, a 62-year-old man from Canton Lucerne lay on the treatment table in the therapy station Gantry 1 and became the first person in the world to receive proton irradiation with the spot-scanning technique. His malignant skin cancer could not be treated and healed with the new method, but the metastases that had formed in his brain stopped growing. This afforded the patient several more years with a good quality of life.
Spot scanning had been developed by PSI researchers, and the first patient treatment was carried out at the institute’s own proton therapy facility. The Center for Proton Therapy CPT of the PSI is, to this day, the only facility in Switzerland where patients with certain cancers can be treated by means of proton beams.
In proton therapy, a proton beam — that is, a concentrated beam of fast-moving protons — kills the tumour cells by destroying their genetic material, their DNA. In comparison to conventional radiation therapy with X-rays, proton therapy has a crucial advantage: It can be precisely determined where in the tissue the protons should unleash their destructive effect. With protons, therefore, it is much easier to kill only the tumour cells and to preserve the healthy tissue around them.
In principle, proton therapy for treatment of cancer patients is much older than 20 years. Already in 1984, tumours in the eye were treated with protons at the PSI. With the development of the spot-scanning technique, it then became possible to treat tumours situated deep within the body more effectively. Since 1996, the number of treatment centres worldwide — ten at the time — has grown more than sixfold, with a continuing upward trend.
When the first patient was treated with the spot-scanning technique at the PSI 20 years ago, it was a milestone in the history of radiation therapy,
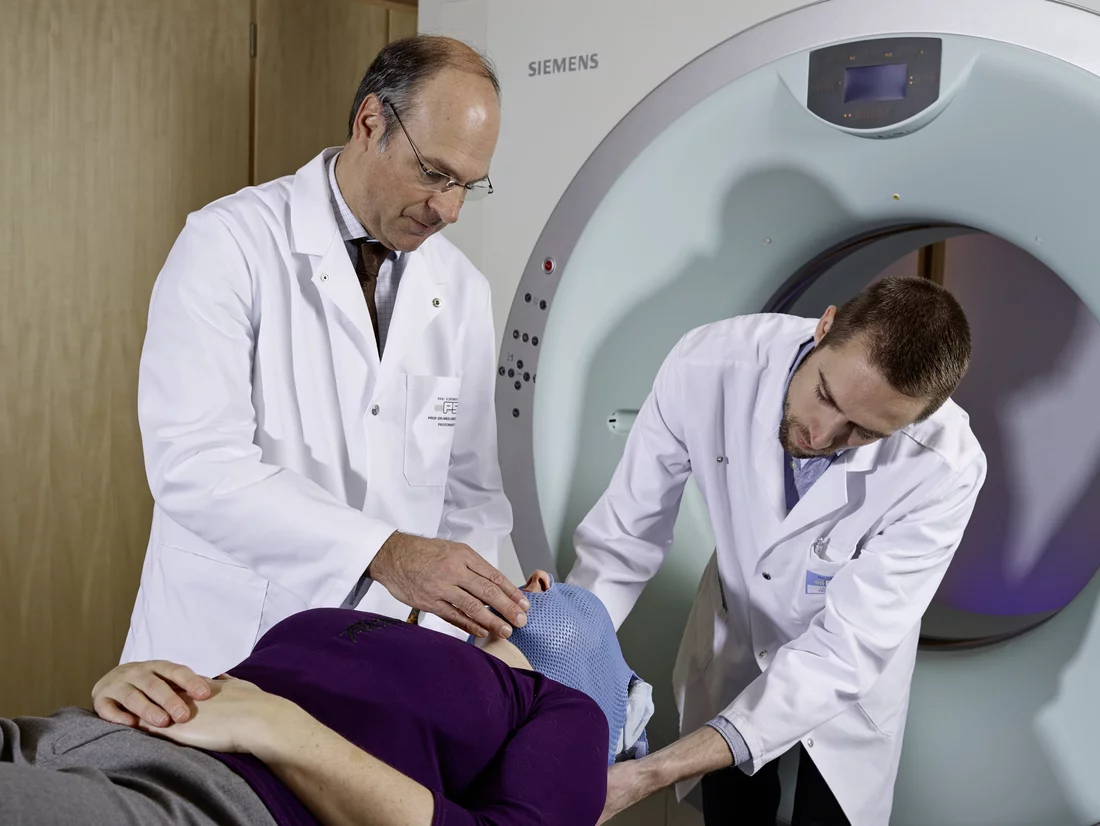
Damien Charles Weber, head and chairman of the Center for Proton Therapy CPT at the PSI, notes with pleasure on the occasion of the anniversary. All the development work for the technology and the treatment facility, right through to the first practical application, took place here at the PSI. That was only possible thanks to the specialised expertise of our staff with respect to radiation physics, as well as with the infrastructure for proton beams at the PSI.
Swiss precision for cancer therapy
First, an accelerator was needed to deliver the proton beam. In 1996, that was the large ring cyclotron then as now serving research at the PSI. Yet for more than ten years now the CPT has had its own system. This cyclotron accelerates the protons to around two-thirds of the speed of light, with which they then fly into a swivelling irradiation machine, the gantry.
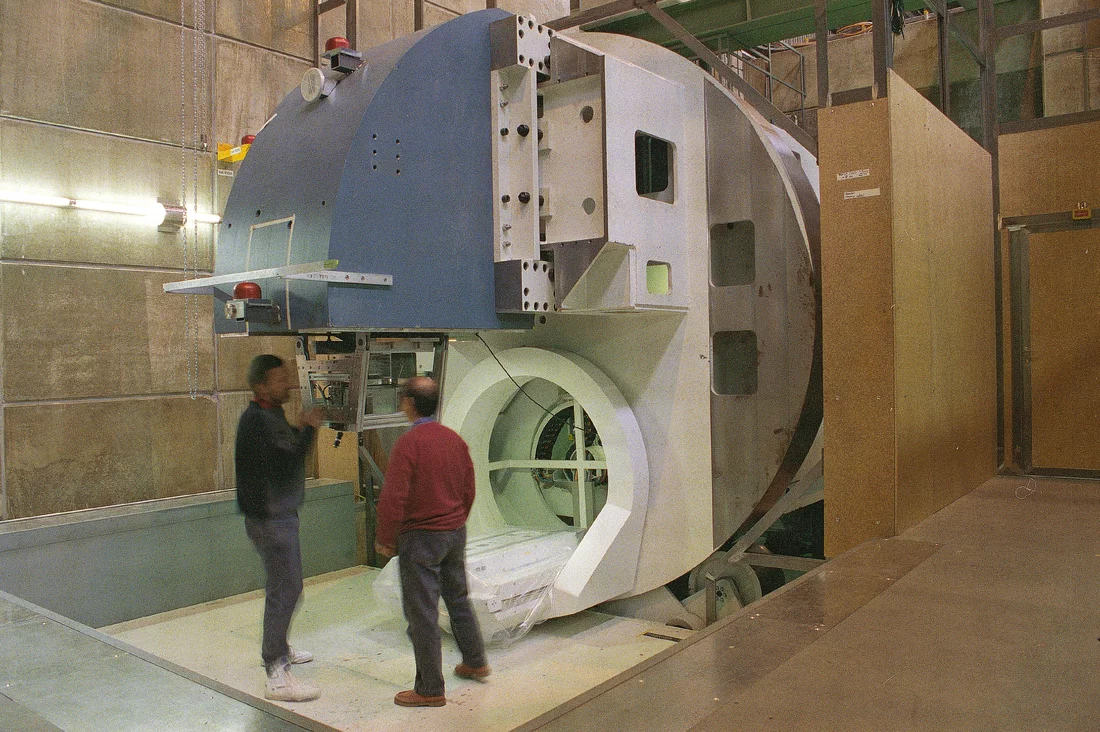
Anyone who has never seen a gantry before is at first struck speechless in the face of the machine’s dimensions,
Weber says, emphasising: Although our first gantry was the size of a lorry, it was the most compact gantry system in the world, and it remains, up to today, absolutely dependable. It works with the precision of a Swiss watch.
Gantry 1 — as the steel colossus is named — was designed entirely at the PSI and was built with help from small and medium-sized Swiss companies. At the head of them all was Schär Engineering AG, which since that time has specialised completely in manufacturing systems for proton therapy. Gantry 1 is a beautiful example of how, again and again, the high technical requirements of the PSI also challenge and advance Swiss industry,
Weber says.
Special advantages for children
So far, more than 1100 patients have been treated at Gantry 1. In addition, CPT has had a second gantry since 2013, and a third is under construction.
Weber and his team most often treat patients with brain tumours and cancers in the ear, nose and throat area. One patient group is especially close to the doctor’s heart: Among the 1200 cancer patients that we have already treated with the spot-scanning technique were 430 children. With them, conventional irradiation should not be used; the risk would be too high. Children can only tolerate a much smaller radiation dose than adults, because their cells are still growing and dividing, which is why they are more sensitive to radiation and can be harmed more easily.
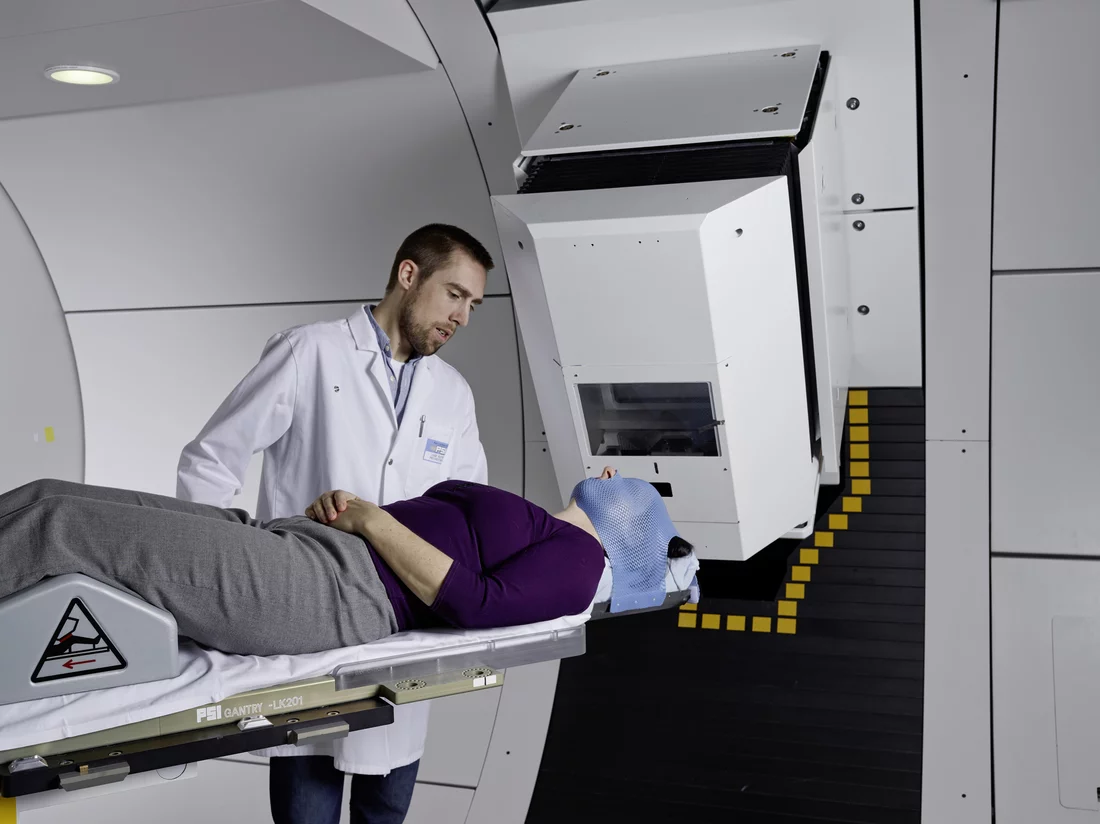
Painting with protons
Specifically for children, the spot-scanning technique has major advantages because it allows for especially precise treatment. In this method, the protons, in the form of a thin particle beam, are fired at the tumour layer by layer, whereby the proton beam scans the tumour from back to front, layer by layer and row by row. It is as if one wanted to fill in the three-dimensional form of the tumour with tiny points. The beam first reaches the deepest layer of the tumour; when this is filled in, the next higher layer has its turn, and so on. It is almost like painting,
Weber finds, in which one first draws the background and then applies ever more layers over it.
For that reason some specialists in this method also call it pencil-beam scanning. By the end of an irradiation treatment, the whole volume of the tumour from back to front has been hit by the beam.
To achieve that, the protons on the one hand must be focused on exactly the right spot and on the other hand must have the right energy, so that they penetrate to the desired depth in the body. With the help of magnets, the beam is concentrated in such a way that it will hit the tumour, point by point, with an accuracy of 1.5 mm. Fine adjustment is done through the shifting of the patient treatment table. To obtain the right penetration depth, the energy of the proton beam must be constantly adjusted. Unchecked, the proton beam releases its energy at a depth of around 40 centimetres below the surface of the body. The shallower the tumour sections to be irradiated lie, the more the proton energy needs to be decreased. This reduction is accomplished through so-called degrader or range-shifter plates — plastic sheets or graphite wedges placed in the beam’s path to absorb part of the proton energy.
Proton irradiation by means of spot scanning has proven its worth particularly for deep-seated, irregular types of cancers. Because this method allows the proton beam to be regulated with high precision, tumours that grow around the spinal cord, the optic nerve, or important organs can now, for the first time, be safely irradiated. Yet proton therapy is expensive and thus not the norm. Health insurance companies only cover the costs for a few types of cancer. Nevertheless, Weber believes in the great potential of the method. We have shown that proton therapy with the spot-scanning technique is safe and effective for a variety of tumours,
the doctor says. In current research projects, he and his team are working to refine the method still further.
Text: Sabine Goldhahn
Contact
Prof. Dr. med. Damien Charles Weber (speaks English and French),Head and Chairman of the Center for Proton Therapy,
Paul Scherrer Institute, 5232 Villigen PSI, Switzerland
Telephone: +41 56 310 55 82 (Ulrike Kliebsch), e-mail: ulrike.kliebsch@psi.ch
Additional information
A) Informations concerning the article- An interview with a patient who was recently treated at the PSI.
- Website of the Center for Proton Therapy at the PSI: https://www.psi.ch/protontherapy/center-for-proton-therapy
- Explanation of the spot-scanning process on the website of the Center for Proton Therapy:
- Background 1: Two kinds of radiation therapy
- Background 2: Proton therapy with the passive scattering technique
- Background 3: Gantry 1
For decades, radiation therapy with high-energy X-rays has been an effective method for treating cancer. Yet the conventional beams not only destroy the tumour cells, but also strike and damage healthy tissue on their way through the body. For this reason, many tumours cannot be treated with as high a radiation dose as is really needed. Therefore more and more doctors are considering irradiation with protons — that is, positively charged particles.
Unlike the X-ray beams in conventional radiation therapy, protons have a precisely limited penetration depth at which they release their maximum energy. Before that, body tissue that the proton beam passes through suffers virtually no damage, and the tissue behind the tumour is spared completely. The method is especially advantageous for treatment of tumours that respond less sensitively to radiation and therefore can only be efficiently destroyed with a high dose of radiation. With proton irradiation, this high dose can be applied to the tumour while preserving the healthy tissue around it. The protons achieve their effect by destroying the genetic material, the DNA, in the tumour cells; as a result the cancer cells can neither grow further nor divide again, and they ultimately die off.
Background 2: Proton therapy with the passive scattering technique
In contrast to the spot-scanning technique, in the older form of proton therapy — passive scattering — protons are fired as one thick beam at the entire tumour. This requires a higher dose of radiation, since the beam must fan out in such a way as to cover the whole tumour at its greatest extent. For each patient a specially made collimator — an individually tailored aperture plate made from copper — must be positioned in the path of the proton beam to form it into a shape that matches the size and contour of the tumour. Still, many protons make their way into the surrounding healthy tissue, since the aperture plate represents the tumour at its largest cross-section. In addition, neutrons can be set free when the proton beam strikes the copper plate. Fast-moving neutrons likewise damage the tissue. Therefore the passive scattering technique is generally used only for very compact, regularly formed tumours that lie close to the surface of the body. The spot-scanning technique, in contrast, is used today in around 90 percent of all proton therapies worldwide.
Background 3: Gantry 1
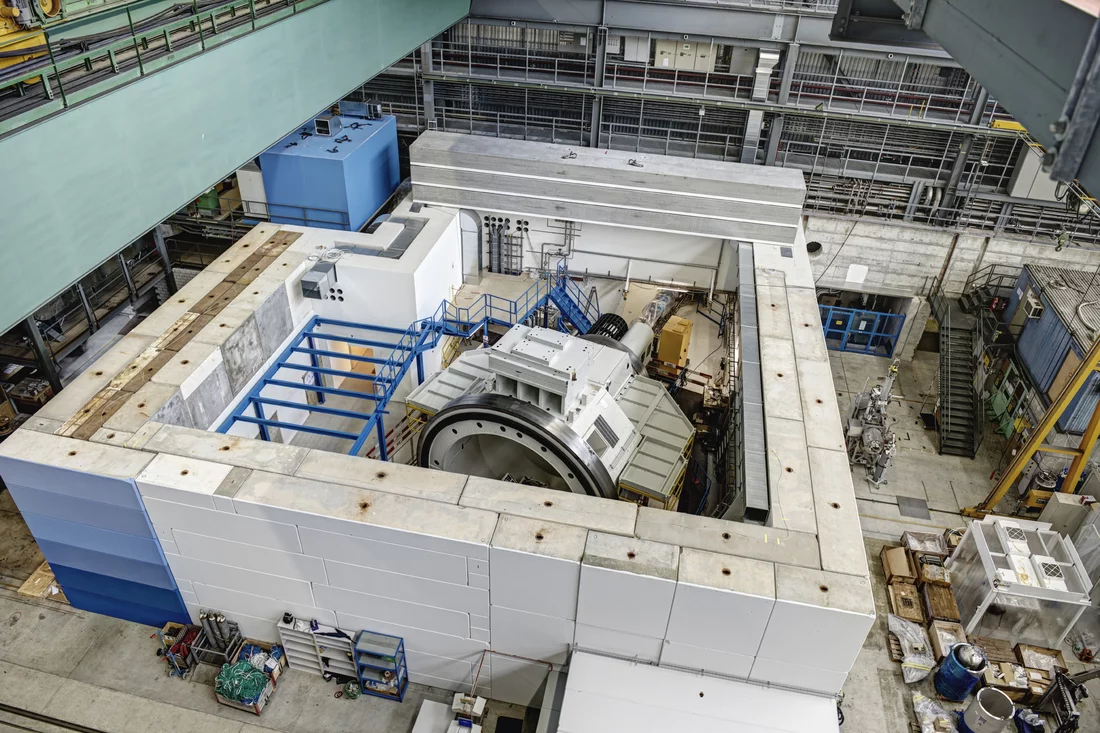
Gantry 1 is the first proton irradiation facility worldwide to function with the spot-scanning technique and is a home-grown development of the PSI. Its physical dimensions are impressive: It weighs 110 tons and has a diameter of four metres. The final section of the beam path, which is carried by Gantry 1, is nine metres long. The gantry is so gigantic because 13 magnets are needed to steer the proton beam from all directions precisely to the patient’s tumour.
One-third of the heavy machine is underground. In the treatment room it looks like an oversized wheel that can turn around its central axis. Gantry 1 can irradiate the patient from any direction and at any angle. Specifically to this end, the floor under the gantry was lowered.
To change the energy of the proton beam and thus its penetration depth, Gantry 1 uses 40 plastic sheets that are suddenly pushed into the beam path shortly ahead of the beam’s outlet port. The patient hears this only as a short click-clack.
B) Further articles about proton therapy
- The article Big help for small children describes how children suffering from cancer are treated with proton therapy at PSI’s center for proton therapy.
- For an overview of the work carried out at the Centre for Proton Therapy (CPT) and the development of proton therapy at the PSI see the article Added value for cancer patients.
- Proton therapy at the PSI started with the irradiation of ocular tumours. To date, the PSI itself has treated 6,700 patients. For more information, please see the article Rays of hope for patients.
- A whole team of specialists is responsible for proton therapy safety and quality standards at the PSI. For details please see Getting a handle on safety.