Radiation therapy using protons is a success story at the Paul Scherrer Institute PSI. For several decades now, doctors have been administering a gentle form of radiation treatment to patients with ocular tumours or those located deep inside the body. Elaborate research carried out at the Centre for Proton Therapy has led to the development of numerous devices, safety systems and software. A radiation method developed by PSI researchers has even resulted in lasting changes in proton therapy worldwide. Despite these successes, researchers at CPT continue tirelessly to refine proton radiation therapy in order to make treatment even faster and more precise in the future.
Antony Lomax really only wanted to stay for two years, carry out intensive research and then return—home to Manchester. But protons exert a special kind of fascination. In particular on medical physicists such as Lomax: A proton is about 1800 times heavier than an electron. That's like comparing a bicycle to a tank. Proton therapy demands not only that we accelerate these heavy particles but also that we target them accurately to within a millimetre of their destination. Protons are a challenge for researchers.
And so, of course, are patients. Every patient and every tumour is different, so there is no single standard treatment for everyone. That is what makes my profession so interesting
, says Lomax enthusiastically. This is why, after 25 years, he is still working at the Centre for Proton Therapy CPT at the Paul Scherrer Institute.
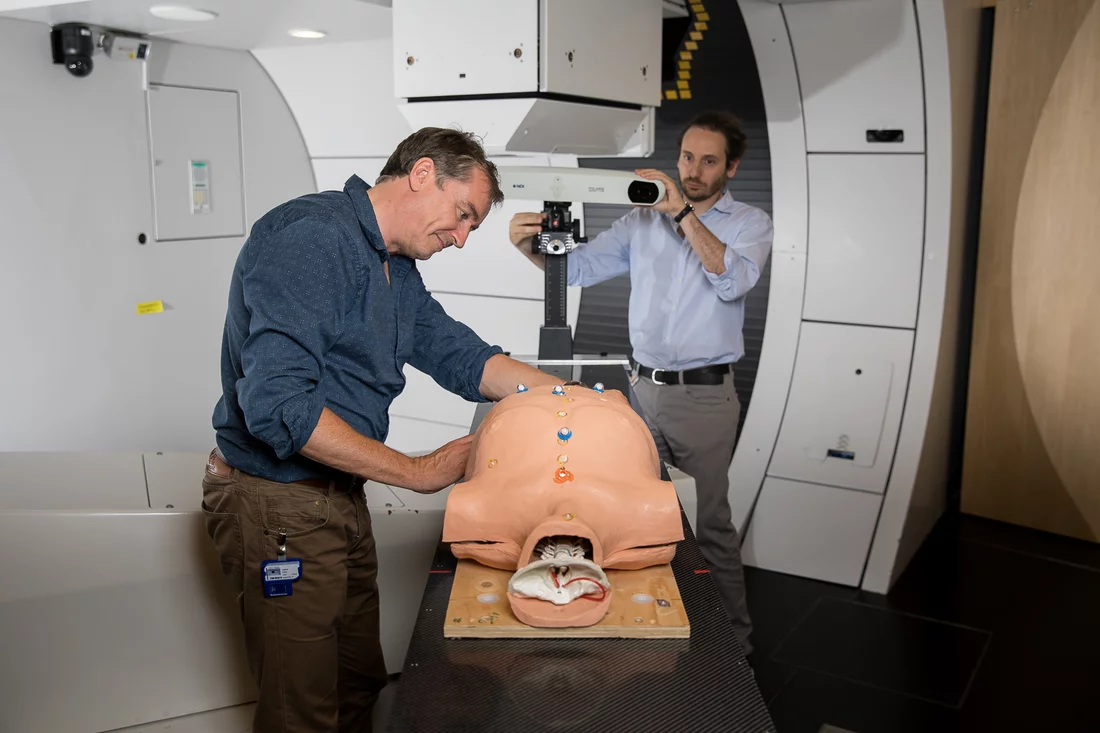
Scientists like Lomax don't like to take it easy, sit back and be proud of what has been achieved in many years of development work. Three treatment rooms are available to patients at CPT. A fourth is in the process of being completed. The so-called spot-scanning technique — a particularly accurate and gentle radiation procedure – was developed here at PSI twenty years ago. Today, doctors world-wide use it to treat cancer. Software specifically developed at PSI ensures accurate planning and implementation of each radiation session. Furthermore, comprehensive safety systems and quality controls guarantee a smooth procedure and highest safety standards. So far, 8000 patients have been successfully treated. Reason enough to be happy with what's already been achieved?
No time for a time-out
After a quarter century at PSI, the medical physicist Lomax sees no reason to relax and sit back: We've had huge successes with our proton therapy. But some thorny problems remain and our current research is dedicated to making proton therapy quicker, safer and usable on movable tumours.
There are organs in the body that are constantly in motion. These include the lungs and liver. Treating tumours in these organs with proton therapy is especially challenging because there is a risk of affecting too much healthy tissues around the tumour. Every breath, every other kind of movement can lead to the tumour moving out of the proton beam's focus. This makes accurate planning difficult.
Normally, medical physicists plan to irradiate tumours located deep inside the body in a way that allows the proton beam to scan the tumour spot-by-spot and layer-by-layer until it has been completely irradiated with a previously calculated radiation dosage. To achieve this result, the tumour must first have been imaged using computer tomography and magnetic resonance imaging and its contours mapped on several dozen millimetre-thin sectional images. Based on these sectional images, the radiation parameters are established: these include beam direction and the individual duration and dosage with which each individual area of the tumour is to be treated. But when the patient breathes, the targeted areas shift by a few millimetres, the calculated radiation plan is no longer completely accurate and healthy tissues can be affected. This is what Lomax and his team intend to avoid by developing various new irradiation techniques.
One of these is referred to as rescanning. This process involves repeated scanning of all points in the tumour by the proton beam. In contrast to earlier practice however, the previously calculated radiation dose is not delivered all at once but in several smaller doses whose intensity depends on the number of times that the proton beam scans a given point. For example: instead of targeting a given spot in the tumour once with the complete dose, it is radiated five times with a twenty percent dose. This approach minimizes the risk of over-radiating a spot in the tumour or missing it completely. Radiation is more evenly applied.
Breathe in, hold breath, switch on the proton beam
Another way of irradiating moving tumours is the so-called breathhold
-technique. This requires patients to hold their breath for several seconds whilst an area in the tumour is being irradiated. But not every patient can hold their breath for twenty seconds or longer. Lomax believes that five to ten seconds is the most that can be expected. And there's another problem: not all patients breathe in to the same depth when holding their breath with the result that the tumour still sometimes moves. This is why scientists have developed another technique referred to as gating
. This method involves using two video cameras to record the chest's movements as the patient breathes in and out and subsequently transferring the images to a computer, which then develops a patient-specific curve similar to a sine curve. The researchers then draw a horizontal line through the curve. At the end of the breathing-out phase and at the beginning of the breathing-in phase, chest movement is less pronounced and lies beneath this line. This is the point at which scientists irradiate. Because people tend to spend longer breathing out, irradiation begins in the second half of the breathing-out phase and continues until the patient begins to breathe in again.
Faster than one breath
Regardless of the technique used: the relatively short breathing phases leave researchers with very little time to irradiate a moving tumour. There is at least one solution that could help here: irradiation would have to be faster, enabling more tumour tissue to be targeted in a shorter time span. But how is this to be achieved?
There are various possibilities for rapid irradiation
, says Lomax. We can increase the beam intensity—the number of proton particles—used during irradiation. This would enable us to increase radiation speed by a factor of two.
The PSI's high-performance particle accelerator could easily manage this. But proton therapy requires more than simply directing the beam at the tumour. The safety systems also have to be adapted accordingly. These measure the dosage and target area during each treatment session in millisecond timespans. In case of error, the beam is automatically stopped. If researchers want to irradiate with a higher intensity, these systems will have to be adjusted and approved by the Federal Office of Public Health. The same applies to a further option, which involves shortening radiation times: line-scanning.
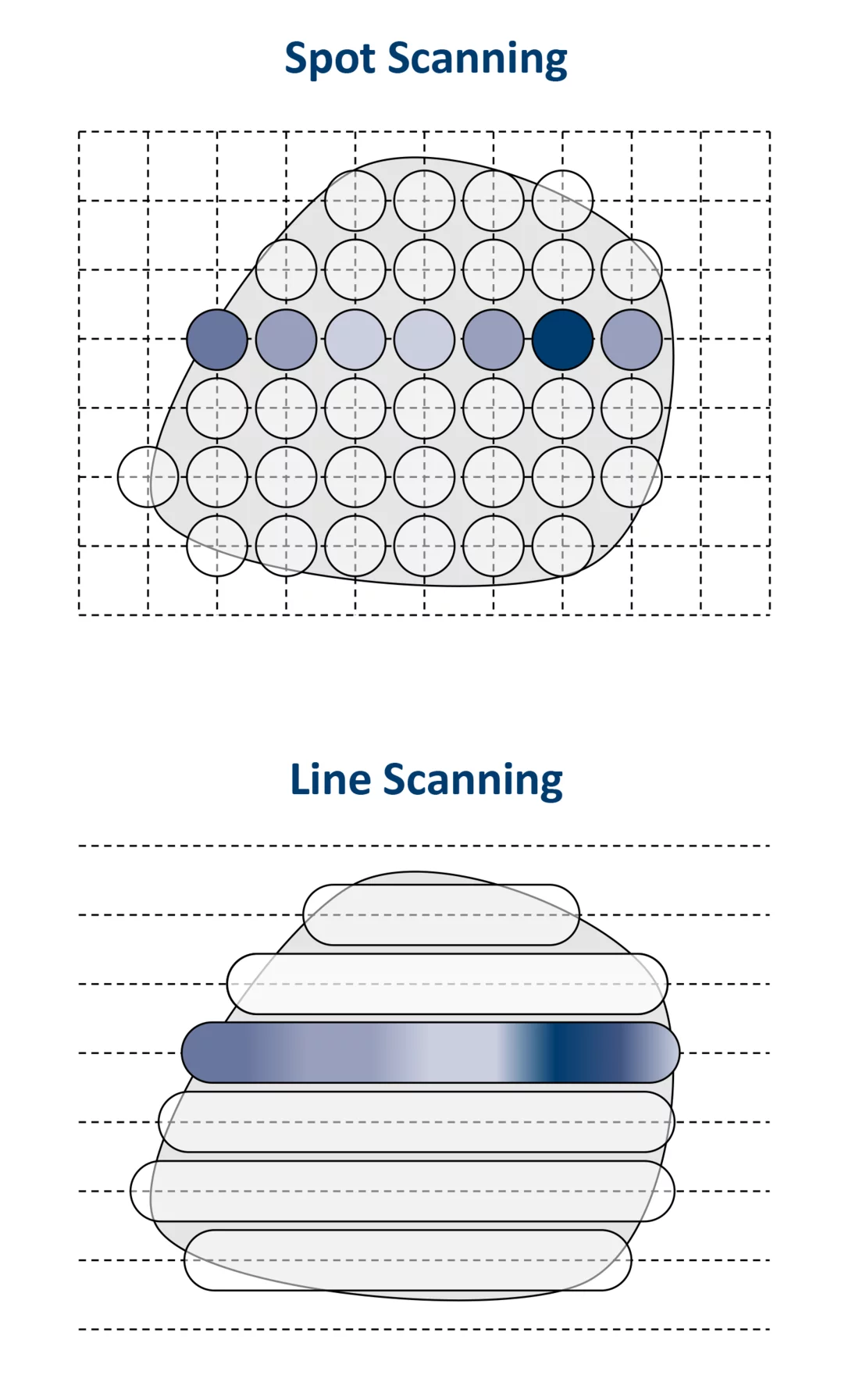
Drawing lines instead of spots
Lomax believes that line-scanning could replace the spot-scanning technique developed at PSI and increase radiation speed by a factor of two. But how will this be achieved? During spot-scanning, the pencil-thin proton beam scans the tumour point by point, as if somebody were filling in the entire volume of the tumour with thousands of pencil dots. After an individual spot has been irradiated, the beam is briefly switched off, moves to the next spot and is then turned on again. The time in between is lost time. The physicists at CPT would like to change that by permeating the tumour not with dots but with continuous lines. The proton beam would no longer have to stop in between but would glide through the tumour like a pencil tracing a line. If we were able to increase radiation speed, the patient would spend less time in the treatment room and more patients could be treated
, explains Lomax.
In addition to working on radiation speed, researchers at the CPT have a number of other exciting projects in the pipeline with which they intend to improve proton therapy. Our techniques work with pin-point accuracy
, says an enthusiastic Lomax, but it's always possible to improve precision and efficiency. And that is what we are working on.
Text: Sabine Goldhahn
Further Information
- For an overview of the work carried out at the Centre for Proton Therapy (CPT) and the development of proton therapy at the PSI see the article Added value for cancer patients.
- The article Big help for small children describes how children suffering from cancer are treated with proton therapy at PSI’s center for proton therapy.
- A special form of proton therapy called spot-scanning technology was developed over twenty years ago at the PSI. This method is now used worldwide and has already helped several thousand patients. Details are provided in the article entitled 20 Years of high-precision combat against cancer.
- Proton therapy at the PSI started with the irradiation of ocular tumours. To date, the PSI itself has treated 6,700 patients. For more information, please see the article Rays of hope for patients.
- A whole team of specialists is responsible for proton therapy safety and quality standards at the PSI. For details please see Getting a handle on safety.
Contact
Prof. Dr. Antony John LomaxChief Medical Physicist at the Centre for Proton Therapy
Paul Scherrer Institute, 5232 Villigen PSI, Switzerland
Telephone: +41 56 310 55 80, e-mail: tony.lomax@psi.ch
Dr. Ulrike Kliebsch
Responsible for Science and Information Services at the Centre for Proton Therapy
Paul Scherrer Institute, 5232 Villigen PSI, Switzerland
Telephone: +41 56 310 55 82, e-mail: ulrike.kliebsch@psi.ch