At the Centre for Radiopharmaceutical Sciences of the Paul Scherrer Institute PSI, scientists are developing new medicines against cancer. These contain radioactive substances that can be injected into the patients and thus make their way to the tumour. There, in direct contact, their radiation should destroy the cancer cells. Before such a radioactive medicine can be tested on patients in the first clinical trials, however, its safety must be guaranteed to ensure that the patient will not be harmed. Therefore every agent is produced at the PSI under sterile conditions and tested – separately for each patient, and only on the doctor's order.
When pharmacist Susanne Geistlich enters her workplace in the PSI laboratory, she disappears into another world. Clothed in a surgical mask, a protective suit and head cover, sterile sleeves, special shoes and safety glasses, she busies herself with small vials containing medicinal compounds. In the background, quietly whirring, is the sound of the ventilation system. Neither germs nor dust particles are permitted to fly around in the air here, because Geistlich's lab is a clean room, with laws of its own. Here the strictest rules apply. But what's the purpose of such an effort?
Here, under the highest purity requirements, the pharmacist and her team develop radioactively tagged drugs and then manufacture these for the first clinical studies in humans. Not, however, in large amounts or for mass production. What is produced here is customised medicine, made to order. Yet neither the medicines nor the requests Geistlich handles are routine, because doctors order radiation of a specific strength for precisely one patient at a time. Here at PSI, we don't manufacture any medicines in quantity,
the pharmacist stresses, but rather produce just one dose for each individual patient participating in a study at exactly the point in time when the doctor needs it.
Time is the most critical factor for every order, because in contrast to conventional medicines, the efficacy of a radioactive drug decreases with every passing minute. For that reason, Geistlich cannot build up supplies in advance but instead has to start fresh every time, carefully processing several components at once: a radiation source that is trapped in a cage
of atoms; a small protein that will transport the radiation to the targeted cells; and a liquid that dilutes this mixture so that it can safely be injected into the blood stream. The finished medicine the patient receives by injection in the clinic contains only one millionth part of the active ingredient. That is no more than a homeopathic treatment with a dilution of D6, or one sugar cube in four metric tons of sugar.
Effective and precise
The radiation in this tiny portion of the medicine originates from radioactive isotopes such as lutetium-177, for example, and is meant to destroy the cancer cells. To this end, the isotopes must first reach the malignant tumour. For this to succeed, they must be coupled to molecules with the ability to transport such isotopes through the blood stream and, following the key-and-lock principle, to dock with cancer cells. Only very few molecules are actually suitable for this. One of them is minigastrin, a hormone-like small protein. It fits perfectly to a surface structure that can frequently be found on cancer types such as medullary thyroid carcinoma or small-celled bronchial carcinoma. Researchers at the PSI have already developed an agent from minigastrin and the radioisotope lutetium-177 to the point where there is hope it can destroy this thyroid cancer without bringing on serious side-effects. Now, in order to make the new medicine safe for humans, we must be able to produce it in such a way that it always possesses the same high quality, the same ingredients, the same quantities, the same purity,
explains the pharmacist Geistlich. Another challenge is that the optimal proportion of the radioactive isotope to the minigastrin has yet to be discovered.
We determine the dosage together with the doctors in the clinic,
Geistlich says. Although the minigastrin's only function in the cancer therapy is as a means of transport, to bring the radiation to the targeted cells in the tumour, it is our limiting factor.
Too much of it can cause hormone-like side-effects such as vomiting. Too little, on the other hand, has the effect that not enough of the radioactive isotope reaches the cancer cells and the treatment does not help. A minimum amount of minigastrin is therefore essential. The real effect of the medicine comes only from the radioactive isotope, however, which is why doctors at the Basel University Hospital want to feel their way toward its optimal dosage in a clinical study. For that purpose, Geistlich and her team at the PSI will couple minigastrin with increasing amounts of the radioactive isotope, step by step, in order to determine the amount of radioactivity that has the best effect. That means as complete an eradication of the cancer cells as possible without excessively harming the rest of the organism. Therefore it is important that the concentrations of the individual substances in the finished medicine and the radioactivity of the isotope are 100 percent right,
the pharmacist emphasizes.
Production on demand
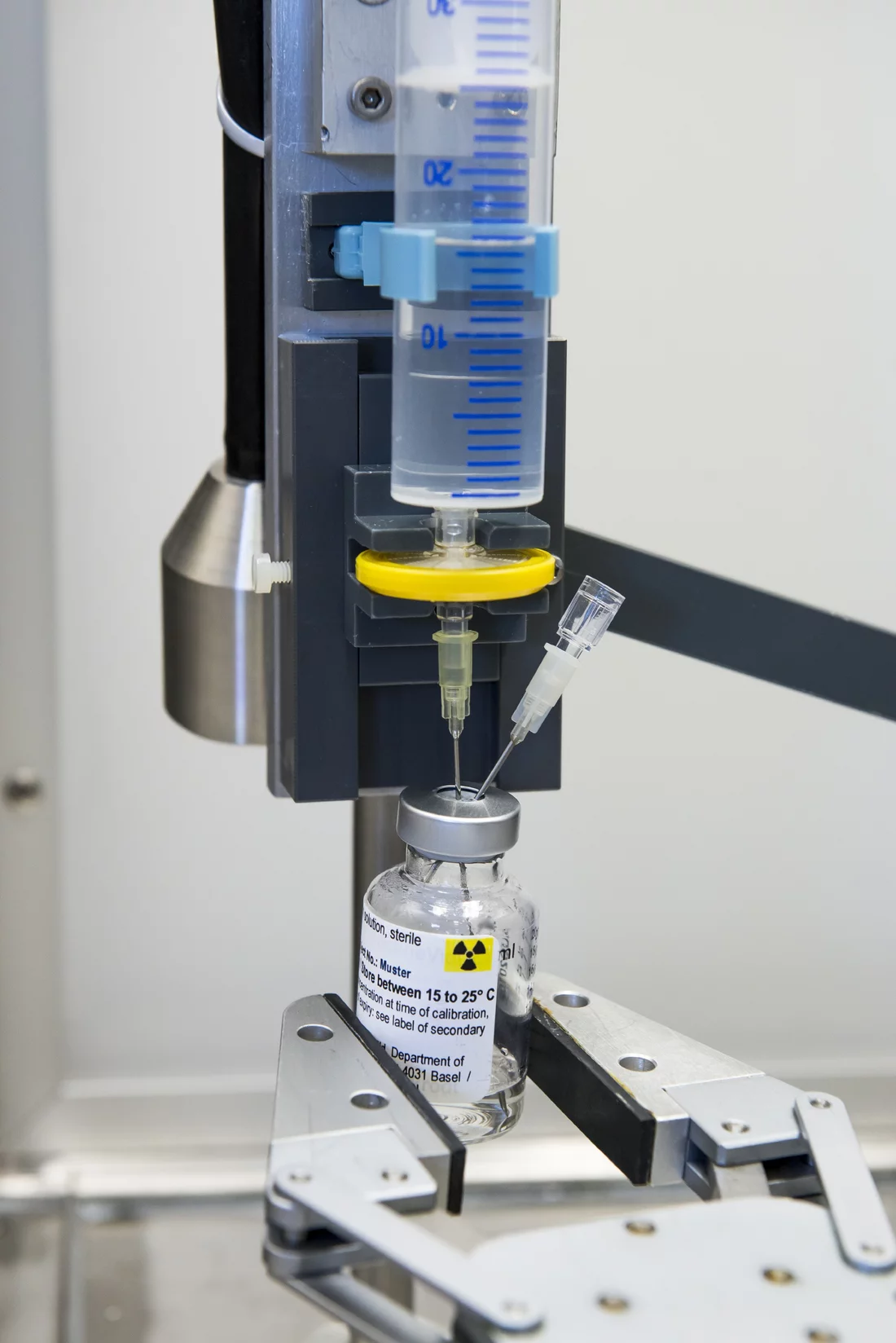
This is where the clean-room laboratory at the PSI comes into play. In the isolated room stands an apparatus in which a large number of hoses and valves connect various reagent glasses and measurement instruments with each other. Its centerpiece is a thimble-sized glass reaction vessel that is shielded by a thick lead sheath: the reactor pot. In it, out of minigastrin and lutetium, Geistlich cooks up the raw product for the radioactive medicine. And in this cooking process, everything must be just right: the ingredients, the duration and the temperature. The mixture of minigastrin and the radioactive isotope can be disturbed by just a tiny amount of contamination by other chemical compounds or a wrong cooking time. If the temperature is too high, on the other hand, free radicals are produced that can change the properties of the medicine. Here a remedy is provided by the antioxidant sodium ascorbate, a relative of vitamin C. That, together with a lower reaction temperature, can raise the yield and increase the purity. Furthermore, the vitamin-C derivative improves the stability – that is the shelf life – of the medicine.
All these details are important and we have checked them three times during the development phase of the new medicine. We need to ensure that the production of the agent is reproducible, always giving the same result in the end,
Geistlich stresses. Again and again, the pharmacist must verify that the production of the radioactive medicine proceeds completely germ-free. Up to now, we have never yet detected bacteria during our production process,
Geistlich says happily, except in the chemical precursors from which the medicine is made in the reactor. They are in fact clean to a high degree, just not sterile.
No more than two bacteria per millilitre are allowed to be in the raw product that emerges directly from the chemical synthesis. Geistlich tests that three times in each case, for every new radioactive agent. After the chemical reaction, the medicine flows through a sterile filter, which catches the last of the germs. Then begins that important step in which the batches of medicine are checked and bottled, sterile, in vials. This sterile bottling process too cannot proceed without verifying, three times, that every individual work step proceeds germ-free. Only with these safety guarantees can the Swiss drug authorisation and oversight agency, Swissmedic, permit the approval of a new radioactive medicine for the first studies with patients.
When finally, after this approval, the call from Basel comes and a patient who is taking part in the study needs his or her radioactive medicine, all of the procedures in the clean room have to be carried out with pinpoint accuracy, from the cooking of the radioactive raw product through the sterile bottling process. In the end, the finished medicine made from lutetium-177 and minigastrin is good for just 24 hours. Only in this short period can one be sure that it will have the desired effect.
If the results of the study with Basel University Hospital show that the radioactive medicine is as effective as the scientists hope, the next steps can be undertaken to further develop it in the direction of a standard treatment of human patients.
Text: Sabine Goldhahn
Additional information
- The following text describes how the drug mentioned in the above article was developed:
Developing a new drug against thyroid cancer
. - The article
Targeting cancer
provides an overview of the work of the Center for Radiopharmaceutical Sciences. - A new method that would channel radioactive substances right into the cell's nucleus is described in the article:
Hitting cancer from the inside
. - The article on how PSI researchers are developing efficient procedures for producing radionuclides used in medical diagnostics:
Designer nuclide for medical applications
. - How researchers at PSI produce radionuclides:
In the focus of the protons
.
Contact
Susanne Geistlich, group leader for Clinical Drug Supply at the Centre for Radiopharmaceutical Sciences at the Paul Scherrer Institute PSI, the ETH Zürich and the Zürich University HospitalTelephone: +41 56 310 28 84, e-mail: susanne.geistlich@psi.ch